Blog 
Click here to go back
Off-Cycle Revalidations

Off-Cycle Revalidations
Provider Enrollment Off-Cycle Revalidations-Skilled Nursing Facilities: Report Expanded Ownership, Management, & Related Party Data
The form CMS-855A has been revised effective October 1, 2024. Beginning on Oct. 1st all SNFs that are initially enrolling, revalidating, reactivating, or undergoing a change of ownership must submit the new form with the new SNF attachment completed.
CMS will revalidate enrolled skilled nursing facilities (SNFs) from October - December 2024 to collect data on ownership, managerial, and related party information. Your Medicare Administrative Contractor will send you a revalidation notice:
• One-third of SNFs will get notices in October
• Two-thirds will get notices in November or December
Click here to view the new Medicare Enrollment Application from CMS.
Click here for additional guidance for SNF Attachment.
Click here for provider enrollment information.
If you need assistance, please contact our office. Call us at (270) 726-4033.
Rhonda Houchens, Director of Operations

Resources: KY Medicaid Ancillary Supplemental Schedule, Beneficial Ownership Information Registry
Kentucky Medicaid Ancillary Supplemental Schedule
As of 7/1/24, Kentucky Medicaid no longer reimburses for ancillaries (Oxygen, PT, OT, SLP, Lab, Xray). Kentucky Medicaid now includes an ancillary add-on $ amount in your Medicaid rate. The ancillary add-on $ amount included in the 7/1/24 rate is based on previously billed ancillary charges. The ancillary add-on will be adjusted every 7/1. As of 7/1/25, the ancillary add-on will be based on a spreadsheet that will be completed and submitted with your Medicaid Cost Report.
Go to Helpful Downloads, Nursing Facility, and they are in the middle of the list.
Click here to view the ancillary schedules and instructions from the Myers and Stauffer website.
Beneficial Ownership Information Registry (BOIR)
Skilled Nursing Facilities: Report Your Expanded Ownership, Management, & Related Party Data
Effective January 1, 2024, many companies in the United States must report information about their beneficial owners—the individuals who ultimately own or control the company—to the Financial Crimes Enforcement Network (FinCEN), a bureau of the U.S. Department of the Treasury.
Who has to report?
• Existing companies: Reporting companies created or registered to do business in the United States before January 1, 2024 must file by January 1, 2025.
• Newly created or registered companies: Reporting companies created or registered to do business in the United States in 2024 have 90 calendar days to file after receiving actual or public notice that their company’s creation or registration is effective.
Who does not have to report?
• Twenty-three types of entities are exempt from beneficial ownership information reporting requirements, including publicly traded companies, nonprofits, and certain large operating companies.
• Small Entity Compliance Guide
Click here to view the Small Entity Compliance Guide.
When do I report?
• If your company was created or registered prior to January 1, 2024, you will have until January 1, 2025 to report BOI.
• If your company is created or registered in 2024, you must report BOI within 90 calendar days after receiving actual or public notice that your company’s creation or registration is effective, whichever is earlier.
What information is needed?
• Name
• Date of Birth
• Address
• The identifying number and issuer from either a non-expired U.S. driver’s license, a non-expired U.S. passport, or a non-expired identification document issued by a State.
Click here to view the U.S. Department of Treasury website.
Click here to file a BOI Report.
Medicaid Quality Incentive Program

Medicaid Quality Incentive Program
For FY2025 (7/1/24) providers received the full provider tax assessment rate of $41.43. This amount is built into the Administration line of your 7/1/24 Medicaid rate.
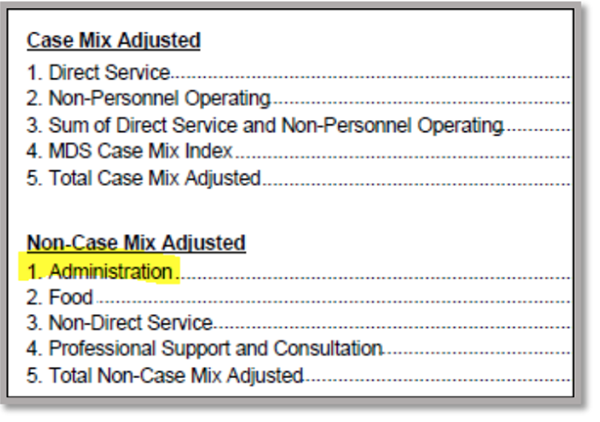
Beginning with FY2026 (7/1/25), the Department for Medicaid Services (DMS) will implement a phase-in of the Quality Incentive Program. The provider tax add-on allowance of $41.43 will be reduced and a quality pool will be created. Providers will earn a quality add-on per diem based on the DRAFT measures below. The highlighted measure is up for discussion.
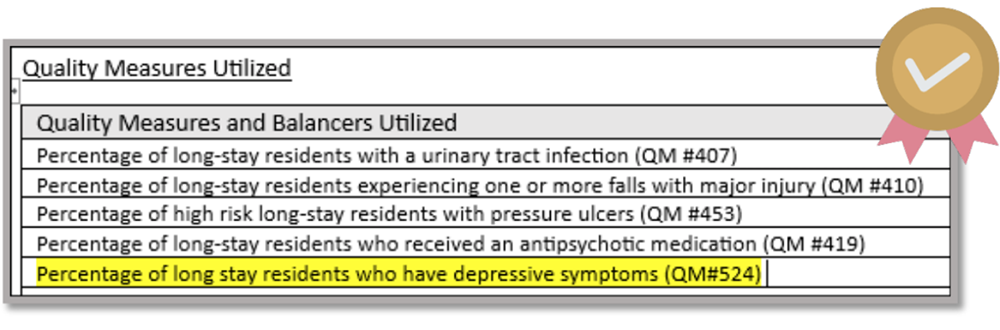
Myers & Stauffer will post a draft Score card of the quality measures in the portal within the next 2 weeks.
Click here to view a printable PDF.
If you need assistance, please contact our office. Call us at (270) 726-4033.
Sarah McIntosh, President

Resources: CMS notifies SNFs of Updates
FFS SNF ABN
CMS revised the SNF ABN, Form CMS-10055, and the form instructions. The SNF ABN form and instructions are located at the link below in the download section. It is available for immediate use, but will be mandatory for use on 10/31/2024.
Click here for complete details.
CMS notifies SNFs: From the latest CMS MLN Connects Newsletter
Skilled Nursing Facilities: Report Your Expanded Ownership, Management, & Related Party Data
CMS will revalidate enrolled skilled nursing facilities (SNFs) from October – December 2024 to collect data on ownership, managerial, and related party information. Your Medicare Administrative Contractor will send you a revalidation notice:
• One-third of SNFs will get notices in October
• Two-thirds will get notices in November or December
You must report this data on the revised Medicare Provider Enrollment Application Form (CMS-855A). We’ll post the revised form and guidance later in September; see Become a Medicare Provider or Supplier.
Click here to view the newsletter.
Kentucky SNF Occupancy Percentage Map, July 2024
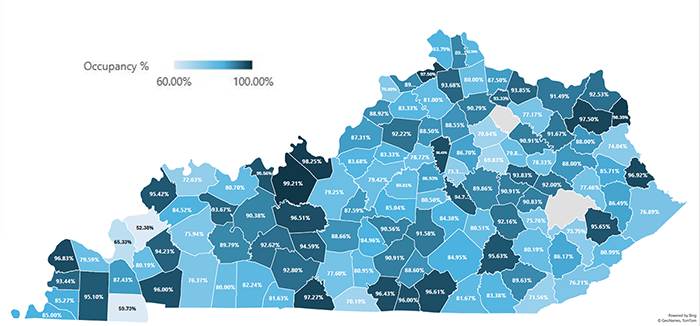
Kentucky SNF Occupancy Percentage Map
July 2024
According to CMS data, the average occupancy for nursing homes in Kentucky is 85.45%.
Click here to view a high quality PDF of the map.
If you need assistance, please contact our office. Call us at (270) 726-4033.
Sarah McIntosh, President

Resources: Annual DDE/PPTN Recertification Is Due, Personal Needs Allowance Increase
Reminder: Annual DDE/PPTN Recertification Is Due
BAs a reminder, each year, providers must recertify each Direct Data Entry (DDE) and Professional Provider Telecommunications Network (PPTN) user's access.
To recertify, complete and fax the Annual DDE PPTN Recertification Form beginning on:
• June 1, 2024 – Home Health & Hospice providers
• July 1, 2024 – Part A providers
• August 1, 2024 – Part B providers
According to our records, several providers have not yet submitted the form. The final deadline is August 31, 2024.
If you don't complete the recertification process timely, we must terminate your DDE/PPTN access. Once terminated, you will need to submit the J15 DDE PPTN Application/Reactivation form to regain access and normal application processing times will apply.
Click here to complete the Recertification Form today.
Personal Needs Allowance (PNA) Increase
Kentucky Medicaid members retain a Personal Needs Allowance (PNA) for personal and incidental needs while under the care for long-term services. As a result of House Bill 6 (RS 2024), the PNA increased from $40 to $60.00 per month effective July 1, 2024.
This increased amount for PNA will be deducted from the LTC member’s gross income when determining the patient liability for Nursing Facilities (NF), Intermediate Care Facilities for Individuals with Intellectual Disabilities (ICF/IIDs), Institutional Hospice (IHP), and Institutional Program of All Inclusive Care for the Elderly (IPACE).
If you have any questions regarding this change, please contact DMS.Eligibility@ky.gov.
Fiscal Year 2025 Skilled Nursing Facility Prospective Payment System Final Rule (CMS 1802-F)
Fiscal Year 2025 Skilled Nursing Facility Prospective Payment System Final Rule (CMS 1802-F)
On July 31, 2024, the Centers for Medicare & Medicaid Services (CMS) issued a final rule updating Medicare payment policies and rates for skilled nursing facilities under the Skilled Nursing Facility Prospective Payment System (SNF PPS) for fiscal year (FY) 2025.
CMS is updating SNF payment policies, which would result in a net increase of 4.2%, or approximately $1.4 billion, in Medicare Part A payments to SNFs in FY 2025. In addition to the SNF PPS rate update, CMS is rebasing and revising the SNF market basket to reflect a 2022 base year. CMS is finalizing several changes to the PDPM ICD-10 code mappings and rule changes to CMS’ enforcement policies to impose more equitable and consistent civil monetary penalties (CMPs) for health and safety violations. CMS is finalizing updates to the SNF Quality Reporting Program (QRP) to better account for adverse social conditions that negatively impact individuals’ health or health care by adding four new social determinants of health (SDOH) items and modifying one SDOH assessment item for the SNF QRP. Additionally, CMS is finalizing a policy requiring SNFs included in the SNF QRP to participate in a process to validate data submitted under the SNF QRP beginning with the FY 2027 SNF QRP. The final rule also contains updates to the SNF VBP program.
7/1/24 Kentucky Medicaid Rate Letters

7/1/24 Kentucky Medicaid Rate Letters
USPS Mailing and Portal Access
Per Myers and Stauffer, hard copies were sent via USPS on Monday, July 22nd. All rate letters will be posted to the Myers and Stauffer portal on Tuesday, July 23rd. Please send your rate letters to our office for review.
The Ancillary add-on calculation is being reviewed by Myers & Stauffer. Stay tuned for updates regarding possible revised rate letters.
If you need assistance, please contact our office. Call us at (270) 726-4033.
Sarah McIntosh, President

Resources: Kentucky Medicaid Changes, PDPM CMI and more
7/1/24 Kentucky Medicaid Changes
Bedhold days reimbursed at a maximum of 30 days per calendar year due to hospitalization.
Bedhold days reimbursed at a maximum of 10 days during a calendar year for leaves of absence other than hospitalization.
ALL Bedhold days reimbursed at 75% of the facility’s rate. Regardless of the SNF census being above 95% or greater for the calendar quarter.
Click here to see Current Regulation 065.
Click here to see Proposed Regulation 065.
Kentucky Medicaid Ancillary Add On as of July 1, 2024
Effective July 1, 2024, ancillary services will be included in the per diem rate calculations and will not be paid outside the per diem rate.
Ancillary services include the following:
• Speech Therapy
• Occupational Therapy
• Physical Therapy
• Oxygen Services
• Laboratory
• X-ray
The ancillary add on will be calculated every July 1. Effective July 1, 2024, the ancillary add on will be calculated as the Medicaid ancillary payments from the prior year divided by Medicaid days. Effective July 1, 2025 and after, the ancillary add on will be calculated as the prior year Medicaid ancillary charges divided by the total Medicaid days, limited to the posted ancillary fee schedule amounts per unit.
Myers & Stauffer will be sending out the final Ancillary Add-on Supplemental Schedule the week of July 29th.
Click here to see Proposed Regulation 065.
PDPM CMI
For rates effective July 1, 2024, the PDPM case-mix index shall be phased in using the following schedule:

Annual DDE/PPTN Recertification
Annual DDE/PPTN Recertification
Each year, providers must recertify each Direct Data Entry (DDE) and Professional Provider Telecommunications Network (PPTN) user's access.
What this means to you:
• Complete the Annual DDE PPTN Recertification Form per the instructions. See link below.
• Fax the completed form to CGS per the timeline below.
The recertification timeline will begin on:
• June 1, 2024 for Home Health & Hospice providers
• July 1, 2024 for Part A providers
• August 1, 2024 for Part B providers
*The final deadline to submit the completed form is August 31, 2024. CGS will deactivate user IDs that aren't recertified on or before August 31, 2024.
FAX to:
Kentucky Part A.........................1.615.664.5943
Kentucky Part B.........................1.615.664.5917
Ohio Part A................................1.615.664.5945
Ohio Part B................................1.615.664.5927
Personal Needs Allowance Increase at 7/1/24 - Has a Few Delays
Personal Needs Allowance Increase at 7/1/24 - Has a Few Delays
As part of House Bill 6, Medicaid is increasing the Personal Needs allowance from $40 to $60. Below is the wording from the House Bill.
• (24) Personal Needs Allowance: Included in the above General Fund 5 appropriation is $3,775,000 in each fiscal year to increase the Personal Needs Allowance 6 from $40 to $60 per month effective July 1, 2024. Notwithstanding KRS 45.229, any 7 portion of General Fund not expended for this purpose shall lapse to the Budget Reserve 8 Trust Fund Account (KRS 48.705). Mandated reports shall be submitted pursuant to Part 9 III, 24. of this Act.
Several SNF’s have noted that the Personal Needs Allowance increase did not occur for all Medicaid recipients. Per Medicaid these changes will be implemented July 22-26.
Kentucky Skilled Nursing Facility Rate Training

Kentucky Skilled Nursing Facility Rate Training
For those who were unable to attend the webinar hosted by Myers and Stauffer on behalf of the Department of Medicaid Services on May 30th, 2024, or for those who would like to review the materials, the recording, slides, and Q&A are available for download. You can access these resources on the Myers and Stauffer, Kentucky Provider page under the Helpful Downloads section, specifically under Nursing Facility.
Click here to visit the Myers and Stauffer website.
Do you have questions? You may call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Sarah McIntosh, President

Resources: Capital Rate Component, Personal Needs Allowance, Scams and CBSA
Capital Rate Component
National Valuation Consultants, Inc (NVC) completed the appraisal process for Kentucky nursing facilities. These reappraisals will be used to determine the facility’s capital component as of July 1, 2024. On average, SNFs are seeing a decrease in their capital rate component of $1. The decrease is related to the inflation factors applied since the 2019 appraisal. There are discussions on how the capital rate components can be calculated differently prior to the next capital rate calculation that will be completed in 2029.
Personal Needs Allowance Increase at 7/1/24
As part of House Bill 6, Medicaid is increasing the Personal Needs allowance from $40 to $60. Below is the wording from the House Bill.
(24) Personal Needs Allowance: Included in the above General Fund 5 appropriation is $3,775,000 in each fiscal year to increase the Personal Needs Allowance 6 from $40 to $60 per month effective July 1, 2024. Notwithstanding KRS 45.229, any 7 portion of General Fund not expended for this purpose shall lapse to the Budget Reserve 8 Trust Fund Account (KRS 48.705). Mandated reports shall be submitted pursuant to Part 9 III, 24. of this Act.
Medical Records Request Scam
CMS identified phishing scams for medical records. This may include scammers faxing you fraudulent medical records requests to get you to send patient records in response. See CMS Medicare Learning Network link below
Click here to see the CMS Medicare Learning Network.
KY Medicaid CBSA changes effective July 1, 2024
907 KAR 1:065 Payments for price-based nursing facility services states that on July 1 of each year, the department shall utilize the most recent Federal Office of Management and Budget’s core based statistical area (CBSA) designations to classify an NF as being in an urban or rural area for Medicaid rate setting purposes.
An updated OMB bulletin no. 23-01 was published July 21, 2023 and will impact nursing facilities July 1, 2024 rates in the following counties:
• Hancock and Henderson will transition from Urban to Rural Status
• Ballard, Carlisle, Lawrence, Livingston, McCracken, and Nelson will transition from Rural to Urban status
If you have questions regarding this please contact our office. (270) 726-4033 or email us at: accountants@hargisandassociates.com
PDPM Resident Roster Reports, Reappraisals & Link to Webinar

PDPM Resident Roster Reports
The 1st and 2nd Preliminary PDPM Roster Reports are available and in your facility’s portal.
Myers & Stauffer Reappraisals
As of 5/24/24, Myers and Stauffer is sending out facility appraisal reports in batches. The remaining batches should be sent by 5/31/24. Be sure to review your appraisals. If you disagree with the output, you have 30 days to appeal.
Myers & Stauffer Webinar
Important Changes are coming to Medicaid Therapy Service Payments
As of 7/1/24, Department for Medicaid Services (DMS) will be paying for therapies (Medicaid only patients) and oxygen as a line item in the Medicaid rate. Myers & Stauffer will be hosting a WEBINAR to discuss the changes.
Thursday, May 30, 2024: 9:30 a.m. - 11:00 a.m. CST, (10:30 a.m. - 12:00 p.m. EST)
We're also excited to share that our very own Sarah McIntosh and Kyle Fritsch will be joining the webinar as panelists! You won't want to miss this important session, as it will be packed full of important information.
Do you have questions? You may call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Sarah McIntosh, President

Resources: (SNF) Value-Based Purchasing Program VBP, Medicaid Personal Needs Allowance Increase
Skilled Nursing Facility (SNF) Value-Based Purchasing Program VBP
The SNF VBP program is a pay-for-performance program. As required by statute, CMS withholds 2% of SNFs’ Medicare fee-for-service (FFS) Part A payments to fund the SNF VBP Program. This 2% is referred to as the “withhold”. CMS is then required to redistribute between 50% and 70% of this withhold to SNFs as incentive payments depending on their performance in the program.
CMS is proposing several operational and administrative proposals as part of this year’s rule. Operationally, CMS is proposing the adoption of a measure retention and removal policy. CMS is also proposing updating the case-mix methodology for the Total Nurse Staffing measure and a review and correction policy update.
Nursing home providers should note that the fiscal 2025 SNF PPS proposal is up for public comment right now through May 28, CMS officials said.
Click here to visit the CMS website to learn more.
Personal Needs Allowance Increase at 7/1/24
As part of House Bill 6, Medicaid is increasing the Personal Needs allowance from $40 to $60. Below is the wording from the House Bill.
(24) Personal Needs Allowance: Included in the above General Fund 5 appropriation is $3,775,000 in each fiscal year to increase the Personal Needs Allowance 6 from $40 to $60 per month effective July 1, 2024. Notwithstanding KRS 45.229, any 7 portion of General Fund not expended for this purpose shall lapse to the Budget Reserve 8 Trust Fund Account (KRS 48.705). Mandated reports shall be submitted pursuant to Part 9 III, 24. of this Act.
J15 DDE PPTN: Application/Reactivation Form
J15 DDE PPTN: Application/Reactivation Form
On February 27, 2024, CGS deployed an online version of the J15 DDE PPTN: Application/Reactivation Form
The online form:
• Allows users a more accurate and efficient process to obtain a User ID for DDE/ PPTN access
• Eliminates errors encountered with the hardcopy form
• Includes an electronic rather than a handwritten signature field A request ID is generated when you submit the application.
If the user(s) is located outside of the United States, please send a copy of the network connectivity diagram to CGS.EDI@CGSadmin.com, and include your request ID in the subject line of the email. Note: CGS will reject paper forms received after March 27, 2024.
CGS DDE/PPTN Recertification Form
Annual DDE/PPTN Recertification
Each year, providers must recertify each Direct Data Entry (DDE) and Professional Provider Telecommunications Network (PPTN) user's access.
What this means to you:
• Complete the Annual DDE PPTN Recertification Form per the instructions. See link below.
• Fax the completed form to CGS per the timeline below.
The recertification timeline will begin on:
• June 1, 2024 for Home Health & Hospice providers
• July 1, 2024 for Part A providers
• August 1, 2024 for Part B providers
*The final deadline to submit the completed form is August 31, 2024. CGS will deactivate user IDs that aren't recertified on or before August 31, 2024.
FAX to:
Kentucky Part A.........................1.615.664.5943
Kentucky Part B.........................1.615.664.5917
Ohio Part A................................1.615.664.5945
Ohio Part B................................1.615.664.5927
Medicaid Timely Filing of Claims

Medicaid Timely Filing of Claims
The Department for Medicaid Services sent a Provider Letter on March 8, 2024, regarding timely filing of claims. The timely filing edit has been suspended for several years and was resumed on 3/8/24. The provider letter mentioned that Medicaid must receive claims no more than 12 months from the date of service. The provider letter did not mention that when the timely filing edit was resumed, coinsurance claims would be affected as well. The timely filing edit for coinsurance claims is 6 months from the Medicare remit date. Just like inpatient claims there will be circumstances when the patient was not Medicaid approved within 6 months or 1 year. If the patient was not approved for Medicaid within 6 months from the Medicare remit date, you will need to submit documentation demonstrating timely filing to Medicaid. Below is the mailing address to submit the timely filing documentation to.
• Claims Submission: P.O. Box 2101, Frankfort, KY 40602-2101
• Coinsurance
• 6 months from Medicare remit date
• Send UB-04, Medicare remit, and Medicaid screen shot to show proof of timely filing.
Do you have questions? You may call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Sarah McIntosh, President

Federal Minimum Staffing Rule Finalized
Federal Minimum Staffing Rule Finalized
CMS is finalizing a total nurse staffing standard of 3.48 hours per resident day (HPRD), which must include at least 0.55 HPRD of direct registered nurse (RN) care and 2.45 HPRD of direct nurse aide care.
Click here to visit the White House website to learn more.
Click here to visit the CMS website to learn more.
Resources: Physician Fee Schedule, Kentucky Medicaid, Medicare Updates and more
Physician Fee Schedule Changes of 3/9/2024
On March 9, 2024, President Biden signed the Consolidated Appropriations Act, 2024, which included a 2.93 percent update to the CY 2024 Physician Fee Schedule (PFS) Conversion Factor (CF) for dates of service March 9 through December 31, 2024.
Click here to visit the CMS website to learn more.
Kentucky Medicaid to Utilize PDPM CMI at 7/1/2024
The Kentucky Department for Medicaid Services will be implementing Patient Driven Payment Model (PDPM) rate methodology effective July 1, 2024. The first Preliminary Resident Listing for 1/1/24-3/31/24 should be available in the Myers & Stauffer web portal at the end of April. Please be watching for this report.
Contact Hargis if you would like us to update your 7/1/24 Projected Medicaid rate with your 1/1/24-3/31/24 PDPM CMI. You may call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Providers Required to Submit Managing Employee Information to Provider Enrollment Records Immediately
This notice provides clarification that SNF providers should not wait for the revalidation to submit any missing medical director or administrator via the Change of Information (COI) submission as soon as possible.
KY Medicaid Reappraisals
National Valuation Consultants, Inc (NVC) has completed the appraisal process for nursing facilities. These reappraisals will be used to determine the facility’s depreciated replacement value. This value will be used to calculate the capital component on the quarterly rates, effective with the July 1, 2024 rate. The NVC reports will be released to Providers by May 31st. If you have questions or need assistance reviewing these reports let us know. All clients, please forward a copy of the reappraisal report to your Client Manager.
Skilled Nursing Facility Prospective Payment System Proposed Rule
For FY 2025, CMS proposes updating SNF PPS rates by 4.1% based on the proposed SNF market basket of 2.8%, plus a 1.7% market basket forecast error adjustment, and a negative 0.4% productivity adjustment.
Click here to visit the CMS website to learn more.
UPDATE: Change to Medicaid Therapy Reimbursement for Medicaid Only Patients
UPDATE: Change to Medicaid Therapy Reimbursement for Medicaid Only Patients
Medicaid reimburses therapy and laboratory/radiology services separately for Medicaid only patients (patients without Medicare B). Department for Medicaid Services (DMS) is tentatively planning to cease reimbursing therapy separately and include therapy as a line item in the 7/1/24 SNF rate.
Also, DMS is tentatively planning to cease reimbursing oxygen separately and include oxygen as a line item in the 7/1/24 SNF rate.
This will be advantageous for SNFs in several ways.
1. Medicaid can pay higher overall rates. The inclusion of therapy increases the Upper Payment Limits.
2. SNFs will no longer have to bill Medicaid for therapies.
3. SNF’s will no longer have to bill Medicaid for oxygen.
4. SNFs will no longer have to obtain therapy prior authorizations.
3. SNF’s will no longer have to obtain oxygen prior authorizations.
Tentatively, the therapy component included in the 7/1/24 Medicaid rate will be based on prior years therapy claims submitted. Starting with the 2024 cost report submission, SNFs will report the therapy provided to Medicaid only patients by therapy discipline, by HCPC, and by month AND oxygen provided to Medicaid patients by HCPC and by month.
Please watch for further updates as the changes become available.
Skilled Nursing Facility Probe and Educate Review

Skilled Nursing Facility Probe and Educate Review
The MLN Matters article, which is linked below, was published in June 2023 announcing Targeted Probe and Educate Reviews (TPE). In the past month, numerous Kentucky SNFs have reported receiving the reviews.
SNF’s will receive a letter in the mail from CSG regarding the TPE. The reviews can be either Pre- Payment or Post-Payment. If your review is Pre-payment, 5 Part A claims will be in a suspended status.
Medicaid will be enforcing the one year timely filing for claims.
Medicaid will be enforcing the one year timely filing for claims.
An Important Memo from the Department for Medicaid Services
The Department for Medicaid Services (DMS) is reminding Nursing Facility Providers (PT12) and Intermediate Care Facilities for Individuals with Intellectual Disabilities (PT11) of requirements related to timely filing. Per federal regulations, Medicaid must receive claims no more than 12 months from the date of service.
For claims 12 months old or more past the date of service to be considered for processing, the provider must submit documentation demonstrating timely receipt by DMS or Gainwell Technologies along with documentation of subsequent billing efforts.
For pending Medicaid members, aged claims may be considered for payment if filed within one year from the eligibility issuance date. A copy of the KY HealthNet card issuance screen must be attached to the paper claim.
HOT TOPICS: Provider Guidance for Medicaid Renewals
Provider Role in Medicaid Renewals
DMS encourages providers to support their patients undergoing renewals in the following ways:
When is their renewal?
Ensure patients know when their renewal due date is and to be on the lookout for notices from KY Medicaid. Encourage them to keep their contact information current in kynect, including mailing address, telephone number and email address.
How to renew?
Guide patients in completing the steps necessary to respond to notices requiring action before their renewal due date. Help them understand what steps to take to upload information. Connect patients to state-employed kynectors, insurance agents, or state-certified navigators for assistance if needed. Providers may utilize content on the KY Public Health Emergency Unwinding website to support understanding of actions to be taken.
What to do if they are administratively terminated?
While the state is taking steps to ensure that this won’t happen, there may be some patients whose coverage ends even though they may be eligible for Medicaid. A lack of providing information or response prior to their renewal due date will lead to DMS being unable to determine eligibility and renew their coverage. For these patients, providers are encouraged to connect these individuals with kynectors, insurance agents, or state-certified navigators to support them in identifying and submitting all necessary materials for redetermination. If done within 90 days after their end date, the patient could be retroactively reinstated without a gap in coverage. Patients also have 90 days to appeal the administrative termination.
What if they are determined ineligible?
For patients discontinued due to no longer being Medicaid eligible, providers may help individuals understand alternative options for health care coverage, including the state’s Qualified Health Plans (QHPs) available at kynect.ky.gov. Connect patients to state-employed kynectors, insurance agents and state-certified navigators to assist.
PHE Renewal Plan
The state anticipates completing renewals for over 1.6 million individuals. The KY Medicaid renewal process will start in April for those individuals with a renewal due by May 31, 2023. DMS will send notices to individuals going through renewals no fewer than 60-days in advance of their renewal date. Through working closely with patients, providers can determine the specific circumstances for their ongoing renewal and support them in understanding the importance of completing the steps required and ways to do so.
Renewals will follow one of three paths:
Passive Renewals.
Medicaid members for which DMS can verify eligibility through existing data sources will be “passively” renewed. Rather than receive a renewal package, individuals who are passively renewed will receive a Notice of Eligibility. Individuals will not be required to take any further action.
Request for Information.
If the state is unable to verify information, an individual may receive a Request for Information (RFI) to support the renewal process. The individual will need to take action by verifying information before eligibility is re-determined.
Active Renewals.
Medicaid members for which DMS does not have sufficient information available to determine the individual’s eligibility will receive a Renewal Packet 60 days in advance of their eligibility review. Individuals will need to take action to upload additional documentation to support re-determining their eligibility.
PHE Renewal Caseload Mix
The caseload of individuals requiring active renewal will be distributed across a 12-month period (May 2023 – April 2024). DMS’ Renewal Distribution Plan has aligned renewal dates for members of the same household as well as aligned Medicaid and SNAP renewal dates.
DMS has prioritized the following populations:
• Medicare-eligible (May to October)
• QHP-eligible (July to April)
• Children under 19 years of age (July to April)
All other populations will be assigned a month for renewal based on the state’s random renewal realignment algorithm. The table below provides the anticipated caseload breakdown, as a percentage of the total population, for the 12-month renewal timeline.

How to Help Patients During the Renewal Process
While working with patients, providers are encouraged to connect their patients to supports in the community to make sure they know how to respond to any notices. There are numerous ways to submit information and many people in the community that can help.

Join Us in Support of Kentucky Nursing Homes by Contacting Your Representatives and Senators

Join us in support of Kentucky nursing homes by contacting your representatives and senators
Kentucky nursing homes are suffering immensely. At this time, 80.16% of nursing homes are AT RISK for financial distress, while 44.53% are ALREADY facing financial distress. This, combined with continued staffing issues and rising costs could mean many nursing homes are at risk for closing across the state.
There are 31 counties projected to be at risk or in distress that contain only one skilled nursing home.
Did you know? There are an average of 210 Kentuckians who are being admitted or readmitted into nursing homes daily.
So, what is the solution?
Join us in support of Kentucky nursing homes by contacting your representatives and senators.
Click here to view the high quality PDF of the graphic above.
Do you have questions? You may call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Sarah McIntosh, President

Resources: Proposed Tax Relief Bill, Screening Risk Change for Skilled Nursing Facilities and Hospice Providers and Medicaid Therapy Reimbursement Changes
Proposed tax relief bill disallows ERC after January 31
The proposed Tax Relief for American Families and Workers Act of 2024 includes disallowing employee retention credit (ERC) claims filed after Jan. 31, 2024. The ERC provision will offset other items in the bill including restoring Sec. 174 (R&E) expensing, enhancements to the child tax credit and other tax relief provisions. It will also allow the IRS to take meaningful action against the pervasive fraud that has plagued the ERC program. While there is a chance that this tax package will not pass and be signed into law, members may want to consider filing any outstanding claims immediately since there is enough Congressional concern about the ERC program that lawmakers could pass a stand-alone bill to end the program early.
Notice of Screening Risk Change for Skilled Nursing Facilities and Hospice Providers
For Skilled Nursing Facilities:
Kentucky Medicaid has been notified of a screening risk level change in 42 C.F.R. § 424.518. for Skilled Nursing Facilities (SNFs) effective Jan. 1, 2023.
As of Jan. 1, 2023, SNFs enrolling or undergoing a change in ownership were elevated from the “limited” level of categorical screening to the “high” screening level. The final rule effectuating this change was published in the Federal Register on Nov. 18, 2022
For Hospice Providers:
Kentucky Medicaid has been notified that effective Jan. 1, 2024, newly enrolling hospices have been elevated from the “moderate” to the “high” screening level.
As of Jan. 1, 2024, Hospice providers enrolling or undergoing a change in ownership shall be elevated from the “limited” level of categorical screening to the “high” screening level. The final rule effectuating this change was published in the Federal Register on Nov. 13, 2023
Additional details can be found on the Department for Medicaid Services website.
Change to Medicaid Therapy Reimbursement for Medicaid Only Patients
Medicaid reimburses therapy and laboratory/radiology services separately for Medicaid only patients (patients without Medicare B). Department for Medicaid Services (DMS) is tentatively planning to cease reimbursing therapy separately and include therapy as a line item in the 7/1/24 SNF rate.
This will be advantageous for SNFs in several ways.
1. Medicaid can pay higher overall rates. The inclusion of therapy increases the Upper Payment Limits.
2. SNFs will no longer have to bill Medicaid for therapies.
3. SNFs will no longer have to obtain therapy prior authorizations.
Tentatively, the therapy component included in the 7/1/24 Medicaid rate will be based on prior years therapy claims submitted. Starting with the 2024 cost report submission, SNFs will report the therapy given to Medicaid only patients by therapy discipline, by HCPC, and by month.
Please watch for further updates as the changes become available.
HOT TOPICS: Provider Role in Medicaid Renewals
Provider Role in Medicaid Renewals
DMS encourages providers to support their patients undergoing renewals in the following ways:
When is their renewal?
Ensure patients know when their renewal due date is and to be on the lookout for notices from KY Medicaid. Encourage them to keep their contact information current in kynect, including mailing address, telephone number and email address.
How to renew?
Guide patients in completing the steps necessary to respond to notices requiring action before their renewal due date. Help them understand what steps to take to upload information. Connect patients to state-employed kynectors, insurance agents, or state-certified navigators for assistance if needed. Providers may utilize content on the KY Public Health Emergency Unwinding website to support understanding of actions to be taken.
What to do if they are administratively terminated?
While the state is taking steps to ensure that this won’t happen, there may be some patients whose coverage ends even though they may be eligible for Medicaid. A lack of providing information or response prior to their renewal due date will lead to DMS being unable to determine eligibility and renew their coverage. For these patients, providers are encouraged to connect these individuals with kynectors, insurance agents, or state-certified navigators to support them in identifying and submitting all necessary materials for redetermination. If done within 90 days after their end date, the patient could be retroactively reinstated without a gap in coverage. Patients also have 90 days to appeal the administrative termination.
What if they are determined ineligible?
For patients discontinued due to no longer being Medicaid eligible, providers may help individuals understand alternative options for health care coverage, including the state’s Qualified Health Plans (QHPs) available at kynect.ky.gov. Connect patients to state-employed kynectors, insurance agents and state-certified navigators to assist.
PHE Renewal Plan
The state anticipates completing renewals for over 1.6 million individuals. The KY Medicaid renewal process will start in April for those individuals with a renewal due by May 31, 2023. DMS will send notices to individuals going through renewals no fewer than 60-days in advance of their renewal date. Through working closely with patients, providers can determine the specific circumstances for their ongoing renewal and support them in understanding the importance of completing the steps required and ways to do so.
Renewals will follow one of three paths:
Passive Renewals.
Medicaid members for which DMS can verify eligibility through existing data sources will be “passively” renewed. Rather than receive a renewal package, individuals who are passively renewed will receive a Notice of Eligibility. Individuals will not be required to take any further action.
Request for Information.
If the state is unable to verify information, an individual may receive a Request for Information (RFI) to support the renewal process. The individual will need to take action by verifying information before eligibility is re-determined.
Active Renewals.
Medicaid members for which DMS does not have sufficient information available to determine the individual’s eligibility will receive a Renewal Packet 60 days in advance of their eligibility review. Individuals will need to take action to upload additional documentation to support re-determining their eligibility.
The caseload of individuals requiring active renewal will be distributed across a 12-month period (May 2023 – April 2024). DMS’ Renewal Distribution Plan has aligned renewal dates for members of the same household as well as aligned Medicaid and SNAP renewal dates.
DMS has prioritized the following populations:
• Medicare-eligible (May to October)
• QHP-eligible (July to April)
• Children under 19 years of age (July to April)
All other populations will be assigned a month for renewal based on the state’s random renewal realignment algorithm. The table below provides the anticipated caseload breakdown, as a percentage of the total population, for the 12-month renewal timeline.

IRS Offers Guidance on Emergency Savings Accounts

IRS Offers Guidance on Emergency Savings Accounts
The Internal Revenue Service provided initial guidance to aid employers in establishing pension-linked emergency savings accounts, an outgrowth of the wide-ranging SECURE 2.0 Act of 2022.
Article by Michael Cohn, AccountingToday.
Do you have questions? You may call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Melodie G Bingham, CPA, Sr. Accountant

Resources: CMS Global PHE and KY Department for Medicaid Services PDPM
CMS Developed Global Public Health Emergency (PHE)
Some denial reasons are as follows:
CMS developed three applications to facilitate visitation and prevent the spread of COVID-19 infection. These one-time grants will continue beyond the PHE to allow all certified nursing facilities access to the products. CNFs can apply for all three programs for up to a total of $9,000.
Communicative Technology: Up to $3,000 for tablets and accessories to allow residents to communicate remotely with family and friends
Visitation I: Up to $3,000 for in-person visitation aids such as outdoor shelters and clear dividers
Visitation II: Up to $3,000 for portable fans and/or room air cleaners with HEPA filters (H-13, -14)
KY Department for Medicaid Services - Patient Driven Payment Model
The Kentucky Department for Medicaid Services will be implementing Patient Driven Payment Model (PDPM) rate methodology effective July 1, 2024. Myers & Stauffer has posted a report to the provider web portal.
The report includes a PDPM Medicaid average CMI for MDS assessments active during calendar year 2022. This is NOT the PDPM CMI that will be used for your July 1, 2024 rate. The report is only a snapshot from 2022 for your facility to use for comparison and rate calculation purposes.
PDPM Medicaid average CMI for rates effective 7/1/2024 will use MDS assessments active between 1/1/2024 through 3/31/2024.
The PDPM methodology will be phased in as follows:

As a reminder, rates effective January 1, 2024 and April 1, 2024 will be based on the 7/1/23 through 9/30/23 CMI. The 7/1/23 through 9/30/23 CMI will also be used during the phase in.
Medicare Program: Appeal Rights for Certain Changes in Patient Status
Medicare Program: Appeal Rights for Certain Changes in Patient Status
CMS has issued a new proposed rule, which would mandate that patients be afforded the ability to appeal hospital reclassifications from inpatient to outpatient status.
The proposed processes would consist of the following:
• Expedited appeals: Proposes appeals for certain beneficiaries who disagree with the hospital's decision to reclassify their status from inpatient to outpatient receiving observation services (resulting in a denial of coverage for the hospital stay under Part A
• Standard appeals: Proposes that beneficiaries who do not file an expedited appeal would have the opportunity to file a standard appeal (that is, an appeal requested by a beneficiary eligible for an expedited appeal, but filed outside of the expedited timeframes) regarding the hospital's decision to reclassify their status from inpatient to outpatient receiving observation services (resulting in a denial of coverage for the hospital stay under Part A).
• Retrospective appeals: Proposes retrospective review process for certain beneficiaries to appeal denials of Part A coverage of hospital services (and certain SNF services, as applicable), for specified inpatient admissions involving status changes that occurred prior to the implementation of the prospective appeals process, dating back to January 1, 2009.
Important Information from Our Call with the Department for Medicaid Services

Call with the Department for Medicaid Services
We recently had a call with the Department for Medicaid Services (DMS) to discuss Medicaid pending issues. We discussed multiple denial issues with DMS and we have been instructed to have providers email the issues to: dfs.medicaid@ky.gov.
If a facility needs to report that someone has been erroneously terminated when they should have been extended, they can email: DMS.Eligibility@ky.gov. ONLY cases where the case should be extended because the member hasn’t responded and they are within the three- month extension period, or it should have been extended because there was a pending state task are to be sent to the DMS email box.
Do you have questions? You may call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Makayla Strode, Accountant

Resources: Kentucky Medicaid Claims and Denials, Therapy Services & KX-Modifiers
Kentucky Medicaid Claims and Denials
Many clients have recently mentioned Medicaid claim denials. Many of the denials are related to the Recertifications process.
Some denial reasons are as follows:
• Patient liability missing on KYMMIS
• Incorrect program code (Managed Care listed vs LTC)
• Incorrect Eligibility Group (Global Choices vs Comprehensive Choices)
While there are multiple denial issues we have been instructed by Department for Medicaid services to have providers email the issues to: dfs.medicaid@ky.gov.
If you are erroneously getting Kentucky Medicaid claims denied with reason code 4227 - “REVENUE CODE IS NOT COVERED FOR THIS MEMBER”, you should email the following to get the Program code fixed: MSServices@ky.gov
Therapy Services
Supervision Policy for Physical and Occupational Therapists in Private Practice Since 2005, we’ve required PTs Private Practices and OTs Private Practices (PTPPs and OTPPs, respectively) to provide direct supervision of their therapy assistants. We’re finalizing a regulatory change to allow for general supervision of therapy assistants by PTPPs and OTPPs for remote therapeutic monitoring (RTM) services, starting January 1, 2024.
KX Modifiers
The KX-modifier threshold amounts for CY 2024 are $2,330 for OT services and $2,330 for PT and SLP services combined.
2024 Kentucky Statewide Appraisals
2024 Kentucky Statewide Appraisals
According to 907 KAR 1:065, Kentucky statewide appraisals are to be completed every 5 years. Beginning January 2, 2024, statewide appraisals will be conducted. As in years past, National Valuation Consultants (NVC) will complete the appraisals. Every Kentucky price-based nursing facility should receive a letter from the Department for Medicaid Services (DMS) regarding the appraisal and the cost.
Kentucky Medicaid Documentation Guidelines

Kentucky Department for Medicaid Services
Myers and Stauffer has posted the 2023 Supportive Documentation requirements effective 10/1/23.
Accuracy of the MDS item responses is very important for many reasons: responses guide the care provided to the resident; Quality Measures assist state survey in identifying potential care problems in a nursing facility; Medicare and Medicaid rates are set based on MDS responses.
These Supportive Documentation Requirements apply to all Kentucky Medicaid-certified nursing facilities that are scheduled for PDPM case mix reviews on or after October 1, 2023.
Myers and Stauffer LC is a certified public accounting firm that provides professional accounting, consulting, data management and analysis services to government-sponsored healthcare programs. Myers and Stauffer LC is a contractor for the Kentucky Department for Medicaid Services.
Do you have questions? You may call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Sarah McIntosh, President

Resources: Kentucky Medicaid, Medicare B Fee Schedule, Training & More
Kentucky Medicaid December Recertifications
DMS is redistributing most renewals in December to other months in the unwinding period. However, there will still be some renewals in December. If a member’s renewal is aligned to another program such as SNAP or TANF, and that program’s renewal is in December, then the Medicaid renewal will stay in December.
Medicare B Fee Schedule Amounts
The Medicare B fee schedules for 2024 have been posted. On average, the fee schedules are decreasing by 3%-4%. Below is a link to CGS website.
Click here to visit the CGS website.
Team Kentucky - Essette Provider Portal / Training
The Cabinet for Health and Family Services (CHFS) Department for Medicaid Services (DMS) has partnered with Gainwell Technologies to implement and maintain a comprehensive Utilization Management (UM) program for Kentucky’s Fee-For-Service (FFS) members.
Altman Z Map

Altman Z Map
The Altman Z-score can be used to predict financial distress within the nursing home industry. Financial variables used to measure liquidity, profitability, efficiency, and net worth are utilized in the calculation.
The Altman Z score considers the balance sheet strength and operational success of a facility. The map below shows the county averages for Kentucky. The scores are calculated using data from the 2022 Medicare cost reports and the modified Altman Z-score from Justin Lord, PHD published in the Journal of Health Care Organization, Provision, and Financing.
Click here to view a high quality PDF of the map.

Do you have questions? You may call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Kyle Fritsch and Leah Shoulders, Directors of Revenue Management


Resources: Kentucky Medicaid Programs and Reminders
Essette Provider Portal
Kentucky Medicaid Utilization Management Program
In June 2023, The Cabinet for Health and Family Services (CHFS) and Department for Medicaid Services (DMS) announced the implementation of a Utilization Management (UM) program for Kentucky’s Fee-For-Service (FFS) members. The new UM program is Essette. Kentucky SNFs will use this program for Prior Authorizations for ancillaries (Oxygen, Physical Therapy, Occupational Therapy and Speech Language). The program is optional to use but will be at the facilities advantage to have an electronic program vs faxing.
The tentative Go Live date is 11/13/2023.
Click here to view the Memo for Trainings and additional information.
Reminder: 30 Days of Bedhold for Kentucky Medicaid
In June 2023, CMS granted approval for Kentucky Department of Medicaid Services to extend the bed hold and bed reserve reimbursement through the unwinding period. Providers will continue to be paid for 30 days of bed hold and 75% of the NF rate if occupancy is less than 95% through the unwinding process.
CMS Improper Payment Probe May Impact Timely Reimbursement for Nursing Homes.

Probe & Education Review Letters
Skilled Nursing Facilities are beginning to receive letters from CMS/CGS regarding the Probe and Educate review process. CMS will have its auditors conduct reviews of five claims per SNF – providers with an error rate of 20% or less will receive education of some kind, while those with an error rate greater than 20% will receive one-on-one education with a Medicare Area Contractor (MAC). MACs were directed to start with providers that show the highest risk. See articles below.
Click here to view the CMS Manual System.
Click here to view the updated Memo from CMS.
Do you have questions? You may call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Leah Shoulders, Director of Revenue Management

Resources: DDE PPTN Recertification Deadline, Prior Authorization Utilization and Kentucky CMI Map
Upcoming Deadline: Annual DDE PPTN Recertifcation
Annual DDE PPTN Recertification Deadline: September 30th
A total of 1,920 DDE/PPTN users did not complete the annual recertification process by August 31st. To ensure DDE/PPTN access is not terminated for these users, CGS is extending the deadline to September 30, 2023. If you still haven't recertified, please complete and submit the Annual DDE PPTN Recertification form today!
After September 30th, CGS must terminate your access. Once terminated, you must submit the J15 DDE PPTN Application/Reactivation form to regain access, and the normal 20 business days for processing applies.
Upcoming Enhanced Prior Authorization/Utilization Management Process
Dear Medicaid Provider,
The Department for Medicaid Services (DMS) is excited to bring the provider community a new platform for requesting and managing prior authorizations for your fee-for-service members. This enhancement is currently slated for early fall and can be accessed by the using the Kentucky Online Gateway (KOG).
In preparation, DMS needs to ensure that the correct provider staff are identified as the Organization Administrator (Org Admin) for the new provider portal where prior authorizations for fee-for-service members will be requested and managed. You have been identified as a current Organization Administrator for a Kentucky Medicaid Provider and DMS requests that you answer the brief survey below. This will help our technical team get the correct staff set up prior to or at the new platform go-live.
Click here to access the survey.
Kentucky CMI Map
Case Mix measures the acuity level of a facility's resident population. The Medicaid Case Mix adjusts the Direct Service and Non-Personnel Operating components of the Medicaid Rate. Effective with the 7/1/23 rates, every .1 increase in Case Mix results in a $9.73 increase in rural Medicaid rates and a $11.48 increase in urban Medicaid rates.
Click here to view a high quality PDF of the map.
Make sure to update your VBP Score.

Make sure to update your VBP Score
As of 10/1/23 the Medicare Rates will be updated. CMS estimates that the aggregate impact of the payment policies in this rule would result in a net increase of 4%. The SNF wage index is different for each urban and rural Core-Based Statistical Area.
While most AR systems update the Medicare rates, they do not update the facility specific Value-Based Purchasing (VBP) score. Each facility must download and update their individual VBP score. If the appropriate VBP score is not entered into your AR system, the AR will not be calculated correctly. The VBP incentive score was frozen at .9920 during COVID. As of 10/1/23, the VBP for each SNF is back in effect. Below are instructions to share with your facility on how to locate this report.
Instructions for Locating your VBP Report
To locate your new report in iQIES, please follow the instructions listed below:
1. Log into iQIES using your Health Care Quality Information Systems (HCQIS) Access Roles and Profile (HARP) user ID and password.
a. If you do not have a HARP account, you may register for a HARP ID using the link below.
2. In the Reports menu, select My Reports.
3. From the My Reports page, locate the MDS 3.0 Provider Preview Reports folder. Select the MDS 3.0 Provider Preview Reports link to open the folder.
4. Here you can see the list of reports available for download. Locate the desired SNF VBP Program Quarterly Confidential Feedback Report.
5. Once located, select More next to your desired SNF VBP Program Quarterly Confidential Feedback Report and the report will be downloaded through your browser. Once downloaded, open the file to view your facility’s report.
For additional questions about accessing your SNF’s report, which can only be accessed in iQIES, please contact the QIES/iQIES Service Center by phone at (800) 339-9313 or send an email to iqies@cms.hhs.gov.
Click here to register for a HARP ID.
For more information about the SNF VBP Program, please visit the CMS website.
Do you have questions? You may call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Resources: Recertify FISS DEE, Form I-9 Updates, Medicaid Errors and Medicaid Rates
Don’t Delay: Recertify Your FISS DDE Access Today!
Have you recertified your Fiscal Intermediary Standard System (FISS) Direct Data Entry (DDE)? The deadline to do so is August 31, 2023.
If you don’t complete the recertification process timely, your FISS DDE access will be terminated. Once terminated, you will need to submit the J15 DDE PPTN Application/Reactivation form and the normal 20 business days to process a new application will apply.
Don’t wait for your access to be terminated.
USCIS to Publish Revised Form I-9
On July 21, U.S. Citizenship and Immigration Services (USCIS) announced they will soon publish a revised version of Form I-9 (Employment Eligibility Verification). The revised Form I-9 (edition date 8/01/23) was published on uscis.gov on August 1, 2023. The agency notes that employers can use the current Form I-9 (edition date 10/21/19) through October 21, 2023. Staring November 1, 2023, all employers must used the new Form I-9.
Click here to visit the USCIS webpage for additional information.
Medicaid Errors with July 2023 Claims
Some SNF’s are having their July Medicaid claims denied due to patient liability. Savannah Wiley at KAHCF has contacted the Department for Medicaid Services (DMS) and they are aware of the error.
DMS stated that the June renewals that were pushed to July are receiving an error with their patient liability as of 7/1. The patient liability is coded as Global Choices vs Comprehensive, and this is causing the July claims to deny.
If you are having this issue, first contact your local office. If the local office is not able to fix this error, email the following and ask them to fix.DFS.Medicaid@ky.gov
Medicare Rates
To receive your final FY 2024 Medicare rates contact one of our accountants today. in order to prepare your SNFs report, we will need to your VBP report and any QRP letters (if applicable).
Do you have questions? You may call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Fiscal Year (FY) 2024 Skilled Nursing Facility Perspective Payment System Final Rule - CMS-1779-F

Fiscal Year (FY) 2024 Skilled Nursing Facility Perspective Payment System Final Rule - CMS-1779-F
On July 31, 2023, the Centers for Medicare & Medicaid Services (CMS) issued a final rule that updates Medicare payment policies and rates for skilled nursing facilities under the Skilled Nursing Facility Prospective Payment System (SNF PPS) for fiscal year (FY) 2024. CMS estimates that the aggregate impact of the payment policies in this rule would result in a net increase of 4.0%. The final rule also includes updates to the SNF Quality Reporting Program (QRP) and the SNF Value-Based Purchasing (VBP) Program for FY 2024 and future years, including the adoption of a measure intended to address staff turnover.
For more information, please visit the CMS website.
Do you have questions? You may call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Rhonda Houchens, Director of Operations

Resources: VBP Report
Instructions for Locating your VBP Report
To locate your new report in iQIES, please follow the instructions listed below:
1. Log into iQIES using your Health Care Quality Information Systems (HCQIS) Access Roles and Profile (HARP) user ID and password.
a. If you do not have a HARP account, you may register for a HARP ID using the link below.
2. In the Reports menu, select My Reports.
3. From the My Reports page, locate the MDS 3.0 Provider Preview Reports folder. Select the MDS 3.0 Provider Preview Reports link to open the folder.
4. Here you can see the list of reports available for download. Locate the desired SNF VBP Program Quarterly Confidential Feedback Report.
5. Once located, select More next to your desired SNF VBP Program Quarterly Confidential Feedback Report and the report will be downloaded through your browser. Once downloaded, open the file to view your facility’s report.
For additional questions about accessing your SNF’s report, which can only be accessed in iQIES, please contact the QIES/iQIES Service Center by phone at (800) 339-9313 or send an email.
Click here to register for a HARP ID.
For more information about the SNF VBP Program, please visit the CMS website.
July 1, 2023 Medicaid Rates

July 1, 2023 Medicaid Rates
Kentucky Skilled Nursing Facilities should be receiving their 7/1/2023 Medicaid rates any time. Medicaid has granted the Price Based Nursing Facilities a 3.0% inflationary adjustment to the price components of the rate, 8.94% increase to the Capital rate component, and a 6.5% “catch-up” adjustment.
Do you have questions? You may call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Debbie Dwyer, Billing Specialist

Resources: Medicare Credit Balance Reports, ABN Form Renewal, Utilization Management and more
Reminder: Medicare Credit Balance Reports Due
As a reminder, the Medicare Credit Balance Report for the quarter ending June 30th is due by July 30, 2023.
ABN Form Renewal
The Office of Management and Budget approved the Advance Beneficiary Notice of Noncoverage (ABN) (Form CMS-R-131 (ZIP)) and instructions (PDF) for renewal. You must use the renewed form with the expiration date of June 30, 2023, beginning August 31. There are no other changes to the form. Visit the ABN webpage for more information.
Click here to download Form CMS-R-131.
Click here to visit the ABN website.
New Kentucky Utilization Management Program
The Cabinet for Health and Family Services (CHFS) Department for Medicaid Services (DMS) has partnered with Gainwell Technologies to implement an automated prior authorization (PA) system for Nursing Facility Ancillary services. The automated PA system will offer a more efficient process that allows a member to begin treatment sooner and allows providers to receive a determination and start services much quicker.
All providers who submit PA requests will need to attend the training. Providers can register for virtual trainings at bit.ly/KYUMTraining. Providers will need to register for a free account and select Provider as your curriculum.
Tentative Go Live date is October 16, 2023.
Click here to view the memo from DMS.
Final MDS 3.0 Item Sets Version1.18.11 v4 Now Available
The final Minimum Data Set (MDS) 3.0 Item Sets version (v)1.18.11 have been updated and are now available in the Downloads section on the Minimum Data Set (MDS) 3.0 Resident Assessment Instrument (RAI) Manual page. The IPA, NP, and SP Item Sets have been replaced with revised versions; the remaining item sets remain unchanged from the last posted version. The MDS Item Sets v1.18.11 will be effective beginning October 01, 2023.
Click here to view the MDS 3.0 Resident Assessment Instrument Manual.
Kentucky - Extension of Bedhold days has been Approved by CMS

Kentucky - Extension of Bedhold days has been Approved by CMS
Veronica Judy-Cecil, Senior Deputy Commissioner reported on June 14th that Kentucky Department for Medicaid Services requested an increase in bedhold days from 14 to 30 AND an increase in bed reserve reimbursement to 75% of the facility's rate if occupancy rate is below 95%.
CMS has granted the approval. The increases will be retroactive to 5/11/23.
Do you have questions? You may call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Rhonda Houchens, Director of Operations

Resources: Section G
Section G
CMS announced last fall section G’s removal from the comprehensive OBRA item set starting October 1, 2023. The removal of this key section from the Minimum Data Set (MDS) will impact the future of nursing home reimbursements by states. Every state is evaluating different methods.
During the Kentucky quarterly meeting of the Nursing Facility Technical Advisory Committee, Kentucky Department for Medicaid Services (DMS) was asked about Section G going away on 10/1. DMS is evaluating the possibilities and researching what other states are going to implement. DMS stated their “goal” is to not have SNFs completing Optional State Assessments (OSA).
We will keep you informed of any updates.
If you need assistance, please contact our office. Call us at (270) 726-4033.
Good News - Increases to our Medicaid Rates!

Good News - Increases to our Medicaid Rates!
Governor Beshear held a press conference yesterday to announce the increase to the 7/1/23 Medicaid rates. After a call with the Cabinet, we have clarification on how the rates increase will be calculated. Medicaid has granted the Price Based Nursing Facilities a 3.0% inflationary adjustment to the price components of the rate, 8.94% increase to the Capital rate component, and a 6.5% “catch-up” adjustment.
If you would like Hargis to calculate your ACTUAL 7/1/23 Medicaid rate, please send the following:
• 4/1/23 Medicaid rate notice
• January thru March 2023 CMI
Please contact our office at (270) 726-4033.
Sarah McIntosh, President

Improper Payment Probe

Improper Payment Probe
All skilled nursing facilities that participate in Medicare Fee-for-Service (FFS) can expect a letter from the Centers for Medicare & Medicaid Services (CMS) regarding improper payment rates starting June 5. CMS will have its auditors conduct reviews of five claims per SNF – providers with an error rate of 20% or less will receive education of some kind, while those with an error rate greater than 20% will receive one-on-one education with a Medicare Area Contractor (MAC). MACs were directed to start with providers that show the highest risk. See articles below.
Click here to view the CMS Manual System.
Click here to view the Skilled Nursing News article.
If you need assistance, please contact our office. Call us at (270) 726-4033.
Sarah McIntosh, President

Resources: COVID-19 Expiration Questions
Questions after the COVID-19 expiration? Our team is prepared and ready!
Due to the pandemic, the healthcare industry has experienced many changes, revisions and addendums the past three years. We know it can cause confusion as you try to work your way through all the changes. We don't want you to miss a deadline or an opportunity to help your community. For your convenience, we have shared important resources below, and as always, our team is available to offer guidance for the expiration of the COVID-19 Public Health Emergency (PHE).
If you need assistance, please contact our office. Call us at (270) 726-4033.
Kentucky Medicaid Renewal Report
As of April 30, 2023, Kentucky nursing facilities and intermediate care facilities will be able to generate a Medicaid Renewal Report listing all individuals with Medicaid Eligibility that are due for Medicaid Renewals.
Click here for the Medicaid Renewal Report for KLOCS Providers.
COVID-19 Notification Requirements
CMS confirmed the requirement to notify all residents and their representatives about COVID-19 cases (F885) ended Monday, May 1, 2023.
Kentucky Medicaid $270 Add-On Ended
Due to the Public Health Emergency (PHE) ending, the last date of service for Revenue Code 550 ($270 COVID-19 add on reimbursement) was May 11, 2023. As of May 12, 2023, claims with Revenue Code 550 will not be paid and providers may need to split the bill for May dates of service.
Resources: 3 Day Stay Waivers, Fiscal Year (FY) 2024 and more
3 Day Stay Waivers end May 11, 2023
The end of the COVID-19 public health emergency (PHE) is May 11, 2023. For resident admissions prior to May 11, 2023, the 3 Day waiver can still be utilized with condition code DR. All admissions after May 11, 2023, will be required to have a 3 day hospital stay to be reimbursed.
Kentucky Medicaid $270 Add-On
Due to the Public Health Emergency (PHE) ending, the last date of service for Revenue Code 550 ($270 COVID-19 add on reimbursement) will be May 11, 2023. As of May 12, 2023, claims with Revenue Code 550 will not be paid and providers may need to split the bill for May dates of service.
Fiscal Year (FY) 2024 Skilled Nursing Facility Prospective Payment System Proposed Rule (CMS 1779-P)
On April 4, 2023, the Centers for Medicare & Medicaid Services (CMS) issued a proposed rule that would update Medicare payment policies and rates for skilled nursing facilities under the Skilled Nursing Facility Prospective Payment System (SNF PPS) for fiscal year (FY) 2024. In addition, the proposed rule includes proposals for the SNF Quality Reporting Program (QRP) and the SNF Value-Based Purchasing (VBP) Program for FY 2024 and future years. CMS estimates that the aggregate impact of the payment policies in this proposed rule would result in a net increase of 3.7%, or approximately $1.2 billion, in Medicare Part A payments to SNFs in FY 2024.
Click here for complete details.
Center of Excellence for Behavioral Health in Nursing Facilities
On the April 13, 2023 CMS SNF/LTC Open Door Forum, an overview of the Center of Excellence for Behavioral Health in Nursing Facilities was shared. We encourage you to review their website and available resources.
Click here to visit the center's website.
CERT Review Contractor name change
The Comprehensive Error Rate Testing (CERT) Review Contractor, formerly known as NCI Information Systems, Inc. changed their company name to Empower AI, Inc.
Advance Beneficiary Notice of Noncoverage: Form Renewal
The Office of Management and Budget approved the Advance Beneficiary Notice of Noncoverage (Form CMS-R-131) for renewal. This renewed form expires January 31, 2026. The expiration date is the only change to the form. You may use the renewed form now, but you must use it beginning June 30, 2023, when the previous version expires.
Kentucky Medicaid Renewal Report
As of April 30, 2023, Kentucky nursing facilities and intermediate care facilities will be able to generate a Medicaid Renewal Report listing all individuals with Medicaid Eligibility that are due for Medicaid Renewals.
Click here for the Medicaid Renewal Report for KLOCS Providers.
Oxygen - Kentucky Medicaid 2023
Oxygen - Kentucky Medicaid 2023
Kentucky Medicaid reimburses SNF’s for approved ancillary billing codes. The ancillary payment methodology is outlined in 907 KAR 1:065, section 12. The current KY Medicaid allowable oxygen procedure codes for skilled nursing facility services are listed below.

Oxygen is reimbursed to the skilled nursing facility based on the durable medical equipment fee schedule. The oxygen fee schedules were updated in Medicaid as of 2/1/23.

If you need assistance, please contact our office. Call us at (270) 726-4033.
Public Health Emergency (PHE) ends on May 11, 2023

Public Health Emergency (PHE) ends on May 11, 2023.
What does this mean for KY Medicaid SNF’s?
• Return to 14 days bed hold days.
• Return to 50% bed reserve reimbursement.
• $270 per diem add-on goes away.
• $29 Rate Add-on DOES NOT go away. The $29 per day Medicaid add-on for Price-Based Nursing Facilities will remain in place until the re-basing occurs.
What does this mean for KY Medicaid recipients with excess resources?
• Kentucky extended the disregard for excess resources for Long Term Care members for 12 months past the PHE. (SPA 22-0012)
Click here to view complete details.
If you need assistance, please contact our office. Call us at (270) 726-4033.
Rhonda Houchens, Director of Operations

Redetermination Date
Redetermination Date
The Kentucky Department for Medicaid Services (DMS) will resume normal operations in alignment with federal laws in May. As part of this effort, DMS will send renewal letters to some Medicaid members beginning in early April 2023 for renewals in May 2023. When the change goes into effect some individuals may be at risk of losing Medicaid eligibility after almost three years of continuous health coverage regardless of changes in their circumstances. DMS' goal is for no one to lose coverage and coordinated efforts are underway to reach all members who will be impacted by this change.
DMS has updated KyHealthNet to include the Redetermination Date for each member.

Medicaid Public Health Emergency Unwinding

Medicaid Public Health Emergency Unwinding
DMS will begin annual renewals for Medicaid members. You may be at risk of losing Medicaid coverage if we cannot reach you. You should update your contact information as soon as possible and keep it updated so Kentucky Medicaid is able to reach you when it is your time to renew!
The renewals will resume in May, but the PHE is still in effect and therefore all the flexibilities that were put in place for providers and members remain in place. When the PHE ends on May 11, 2023, some of these flexibilities will be discontinued (or unwound) and some will continue based on state policy changes.
The Kentucky Department for Medicaid Services (DMS) will resume normal operations in alignment with federal laws in May. As part of this effort, DMS will send renewal letters to some Medicaid members beginning in early April 2023 for renewals in May 2023. When the change goes into effect some individuals may be at risk of losing Medicaid eligibility after almost three years of continuous health coverage regardless of changes in their circumstances. DMS' goal is for no one to lose coverage and coordinated efforts are underway to reach all members who will be impacted by this change.
Please update your information as soon as possible!
Visit kynect.ky.gov or call kynect at 855-4kynect (855-459-6328) to update your mailing address, phone number, email and other contact information. Kentucky Medicaid will then be able to reach you when it is your time to renew!
Click here to view complete details.
If you need assistance, please contact our office. Call us at (270) 726-4033.
Sarah McIntosh, President

KY Public Health Emergency (PHE): Renewal Process
KY Public Health Emergency (PHE): Renewal Process
The Public Health Emergency (PHE) will end 5/11/23. Ky Medicaid will start the renewal process back. Renewals dated 5/31/23 will be the first renewals.
While on 3/22/2023 Ky PHE Stakeholder call, it was mentioned that the renewal dates will be published in KyHealthNet. By March 25, 2023, KyHealthNet will reflect the updated renewal dates for all members. The renewals dates can be viewed under the Members eligibility section.
Click here to stay updated with the renewal process.

Oxygen Prior Authorizations Common Denials
Several SNF’s have recently had issues with Medicaid denying their oxygen Prior Authorizations. After conversations with Carewise, there are a couple of main denial reasons and suggestions to correct.
The most common denial is “not returning information requested”.
• Once the SNF faxes the prior authorization form to Carewise, they have up to 15 days to respond. Carewise’s normal response time is 5-6 days. A Lack of Information (LOI) letter is mailed to the patient address on file in kymmis. The LOI letter gives 14 days for the SNF to gather the information and get it submitted. This poses a major issue for the SNF’s that never receive the letter and do not know anything else is needed. Carewise has given a solution to this problem. The LOI letters are in Ky Health Net. Also, the SNF can call and inquire about the LOI letter. The number is 1-800-292-2392.
Another common denial is “more current MD order for oxygen”.
• Carewise has stated that the monthly order signed by the physician every other month is sufficient for this request. Carewise has also stated that a verbal order from the physician is acceptable if the SNF notes this process was completed.
Another common denial is “provide qualifying room air oxygen saturation levels”.
• Carewise must receive documentation for the patient’s Room Air AND Oxygen usage. Carewise will accept MARS, TARS, and Nursing Notes.
Kentucky Medicaid Update: Member Renewals

Kentucky Medicaid Update: Member Renewals
An important message from The Department for Medicaid Services’ (DMS).
Kentucky will resume normal enrollment and eligibility operations for Medicaid in alignment with federal laws on May 1. After that date, some Medicaid members who have continuously received benefits during the Public Health Emergency may be at risk of losing Medicaid if they are no longer eligible. The Department for Medicaid Services’ (DMS) goals are to reduce unnecessary loss of coverage for those who are eligible and to support those who are no longer eligible in obtaining alternative coverage.
Coordinated efforts are underway to reach all members who will be impacted by this change.
Medicaid renewals will be processed over the course of 12 months. DMS will notify members about 60 days in advance of their renewal date through multiple forms of communication, including letters, text, and email. As a partner of DMS, there are very important ways that you can help support members through their renewal:
• Encourage individuals to keep their contact information updated through their account in kynect.
• Make sure members know to check for any letters, emails, or messages from Medicaid about their renewal status.
• Help members understand the importance of logging into kynect and completing all steps for their renewal.
DMS launched MedicaidUnwinding.Ky.gov to share all information and resources regarding Medicaid renewals and the unwinding of the Public Health Emergency, which will end on May 11, 2023. We encourage you (and your stakeholders) to use this website to access available communications and resources DMS developed to inform the public about the upcoming changes.
We will be holding stakeholder meetings in March to keep everyone informed. More information and invitations to those events will be made available over the next month. DMS will provide regular updates on its social media accounts, so be sure to sign up to stay informed!
Click here to view complete details.
If you need assistance, please contact our office. Call us at (270) 726-4033.
Sarah McIntosh, President

Resources: iQIES, KLOCS Updates and more
iQIES for Minimum Data Set (MDS) Submission Release on April 17, 2023
CMS is excited to announce that the transition of the Minimum Data Set (MDS) assessment submission and reporting functionality to the Internet Quality Improvement and Evaluation System (iQIES) will occur on Monday, April 17, 2023.
To properly prepare for the transition, the QIES Assessment Submission and Processing (ASAP) system for MDS submissions will be turned off on Thursday, April 13 at 8:00 p.m. ET. Providers should submit completed MDS records prior to 8:00 p.m. ET on April 13th to QIES (ASAP) or wait until 8:00 a.m. ET on April 17th to submit data in iQIES. Providers are expected to take into account all requirements when determining the date they submit completed MDS records, including but not limited to, submission timeliness, claims processing, and care planning requirements.
CMS will provide additional information through various email notifications regarding training, technical guidance, details on what to expect, and more.
Register for an iQIES Account
Please note that failure to obtain access to iQIES prior to April 17, 2023 will impact your ability to submit MDS records. As mentioned in previous communications, nursing home and swing bed providers who are required to submit data to CMS must have at least one staff person assigned and approved as the facility Provider Security Official (PSO), who works for the provider and is responsible for approving all other users for their facility. For information and instructions to register for an iQIES account, please visit the link below.
iQIES Service Center
If you have questions or require assistance, please contact the iQIES Service Center at iqies@cms.hhs.gov or by phone at (800) 339-9313. Please note that call volume may be higher than normal during this time.
Click here to register for an iQIES account.
KLOCS Updates to the CHOW Process
Update on how active Level Of Care (LOCs) and applications will be processed when a Change Of Ownership (CHOW) is processed in KLOCS, for Long Term Care (LTC) facilities, as reported by Provider Enrollment.
Starting Sunday, February 5, 2023 – When a CHOW is reported (to KLOCS), saved applications which are associated with the old Provider Number will be withdrawn. Providers impacted by the CHOW will receive a notification in the Message Center indicating which applications were or were not (including a reason) processed by the CHOW. Providers must review the notification and complete any actions identified in the message.
CMS Proposal Marks Shift After Years of Skilled Nursing Frustration with Medicare Advantage Diversion
The Centers for Medicare & Medicaid Services (CMS) has decided to take action on transitions in care – specifically Medicare Advantage (MA) plans diverting care to home health instead of skilled nursing – after years of skilled nursing industry and consumer feedback. CMS has taken steps to address the trend with a proposed rule.
Click here for complete details.
Resources: CMS Proposal and Medicare Enrollment
CMS Proposal Marks Shift After Years of Skilled Nursing Frustration with Medicare Advantage Diversions
The Centers for Medicare and Medicaid Services (CMS) has decided to take action on transitions in care – specifically Medicare Advantage (MA) plans diverting care to home health instead of skilled nursing – after years of skilled nursing industry and consumer feedback. CMS last month took steps to address the trend with a proposed rule
Medicare Enrollment in PECOS: Faster and Easier Application Process — Coming Summer 2023
PECOS system allows registered users to securely and electronically submit and manage Medicare enrollment information. Starting in the summer of 2023, PECOS will add additional features to better serve your needs.
Some of the features will be as follows:
• A single application for multiple enrollments
• Pre-population of data and an application that’s tailored to you
• Enhanced capability to add or delete group members
• Real-time processing checks and status updates
• Re-validation reminders
The 2023 Tax Filing Season has Begun

The 2023 Tax Filing Season has Begun
The IRS recently announced January 23rd as the official start date to the 2023 tax filing season. The announcement includes key filing season dates, tips to help people with the 2023 tax season, free e-file dates, when you should expect your refunds and more important processing topics. For more information see the announcement at the link below.
If you have tax filing questions or are interested in finding out more about our tax services contact one of our tax specialists today.
Click here to view complete details.
If you need assistance, please contact our office. Call us at (270) 726-4033.
Melissa Roberts, Tax Accountant

Medicare Desk Review of Bad Debt Listings
Medicare Desk Review of Bad Debt Listings
Bad Debt Listings are subject to various levels of review during the desk review or audit process.
The completion of review and type of review is dependent on thresholds defined by CMS.
For the 12/31/21 Medicare Cost Reports desk review process, CGS is requesting additional documentation on the Bad debt listings for selected SNFs. The list of items CGS is requesting includes, but isn’t limited to,
• bad debt policy
• bad debt recovery policy
• remittance advices
• proof of write off
• and patient liability verification
Please make sure that you are completing your bad debt log accurately and retaining corresponding documentation. Please contact our office if you would like to discuss. Call us at (270) 726-4033.
Resources: Form Changes, PHE Updates, Medicare Adjustments and more
CMP Grant Opportunities Available
For information on the CMP Reinvestment Fund and the COVID-19 Emergency CMP grants, as well as links to the applications, please view the links below for the KY CMP Information Brochure or visit Civil Money Penalty Funds - Cabinet for Health and Family Services (ky.gov).
Click here to view the KM CMP Information Brochure.
Click here to visit the Team Kentucky website.
Businesses have Feb. 1 deadline to provide Forms 1099-MISC and 1099-NEC to recipients
Redesigned Form 1099-MISC
The IRS revised Form 1099-MISC for the 2020 tax year to accommodate the creation of a new Form 1099-NEC. The redesigned 1099-MISC has different box numbers for reporting certain income. Businesses must send Form 1099-MISC to recipients by February 1, 2021, and file it with the IRS by March 1 (March 31 if filing electronically).
If businesses are using Forms 1099-MISC to report amounts in box 8, Substitute Payments in Lieu of Dividends or Interest, or box 10, Gross Proceeds Paid to An Attorney, there is an exception to the normal due date. Those forms are due to recipients by February 16, 2021.
New Form 1099-NEC
Form 1099-NEC is a new form for tax year 2020 for non-employee compensation of $600 or more to a payee. This form should be filed with the IRS, on paper or electronically, and sent to recipients by February 1, 2021.
There is no automatic 30-day extension to file Form 1099-NEC. However, an extension to file may be available under certain hardship conditions. Also, non-employee compensation may be subject to backup withholding if a payee has not provided a taxpayer identification number to the payer or the IRS notifies the payer that the Taxpayer Identification Number provided was incorrect.
Click here for complete details www.irs.gov.
HHS extends Public Health Emergency from April 11
The PHE renewal through mid-April provides for the uninterrupted continuation of several flexibilities that have protected beneficiary access to important services in as safe and effective manner as possible.
HHS will also continue to waive the three-day hospital stay rule that causes many seniors to be strapped with out-of-pocket costs in the thousands because they do not qualify for Medicare coverage. AHCA continues to advocate to eliminate this confusing and devastating policy barrier altogether.
Click here for complete details.
2023 Medicare Parts A & B Premiums and Deductibles 2023 Medicare Part D Income-Related Monthly Adjustment Amounts
On September 27, 2022, the Centers for Medicare & Medicaid Services (CMS) released the 2023 premiums, deductibles, and coinsurance amounts for the Medicare Part A and Part B programs, and the 2023 Medicare Part D income-related monthly adjustment amounts.
Click here for complete details.
UHC will require electronic submission of claims 1/1/2023.
What are your submission options?
With Optum Intelligent EDI, facilities will have access to submit files electronically, manually key claims, search remits and eligibility.
What will you need?
• One Healthcare ID
If you do not have a current ID you will need to register here: Create One Healthcare ID - One Healthcare ID.
Follow the step linked below to request the Intelligent EDI tool to be added to your United Healthcare Provider Portal Dashboard.
2023 Medicare Physician Fee Schedule Final Rule

Calendar Year (CY) 2023 Medicare Physician Fee Schedule Final Rule
On November 01, 2022, the Centers for Medicare & Medicaid Services (CMS) issued a final rule that includes updates and policy changes for Medicare payments under the Physician Fee Schedule (PFS), and other Medicare Part B issues, effective on or after January 1, 2023. With the budget neutrality adjustments, which are required by law to ensure payment rates for individual services don’t result in changes to estimated Medicare spending, the required statutory update to the conversion factor for CY 2023 of 0%, and the expiration of the 3% supplemental increase to PFS payments for CY 2022, the final CY 2023 PFS conversion factor is $33.06, a decrease of $1.55 to the CY 2022 PFS conversion factor of $34.61.
Many are advocating reductions be delayed. If the rule is implemented as is, Providers will likely see around a 4.5% reduction in Part B payments; 3% from the removal of the supplemental increase and another 1.6% from budget neutrality adjustments.
Click here to view complete details.
If you need assistance, please contact our office. Call us at (270) 726-4033.
Sarah McIntosh, President

Action Required: Register for an iQIES Account
Action Required: Register for an iQIES Account
The Quality Improvement and Evaluation System (QIES) is being upgraded to make the system more reliable, scalable, secure, and accessible. The enhanced Internet-facing, cloud-based system, referred to as the Internet Quality Improvement and Evaluation System (iQIES), aims to reduce provider burden and enhance the ability for the Centers for Medicare & Medicaid Services (CMS) to better serve our community. CMS is excited to announce that we are preparing to release the iQIES for Minimum Data Set (MDS) submission in early 2023.
To gain access to the iQIES system, all users must create an account and establish credentials in the HCQIS Access Roles and Profile (HARP) system, which is a secure identity management portal provided by CMS. To learn more about HARP, click the HARP link below under Resources to review Frequently Asked Questions.
Register for iQIES Access
To receive access to iQIES, please complete the following steps below.
1. Create an account in the HARP system using your corporate email address at the link below. Note: HARP User IDs cannot be adjusted. As such, please refrain from using facility names or any special characters (such as # or &) when creating the HARP User ID. *If the facility handles 2 or fewer providers and does not have a corporate email domain, a personal email address may be used.
Click here to create an account.
2. Access iQIES at the link below and log in with your HARP credentials (completed in step 1) to complete the process to request your User Role for your specific provider CMS Certification Number (CCN).
Click here to access iQIES.
3. Once the user role request has been submitted AND approved by the PSO, you will receive notification via email informing you that your iQIES account access request has been approved.
*IMPORTANT: If your organization has not yet identified and registered a Provider Security Official (PSO), you will not be able to complete a user role request. At a minimum, at least one PSO needs to be registered for each provider, but CMS highly recommends at least two PSOs are designated so there is a higher likelihood someone will be available to approve/reject iQIES access requests. The PSO must work for the provider and cannot be a vendor.*
Note:
Please refer to the following iQIES documents for more information by visiting: https://qtso.cms.gov/software/iqies/reference-manuals
• iQIES Onboarding Guide for step-by-step instructions to request a user role
• iQIES User Role Matrix for a listing of user category descriptions and role privileges
Although the MDS submission functionality will not be available immediately, we strongly encourage users to request access to iQIES as soon as possible, as doing so will allow for a smoother transition prior to the go live date.
Note:
Currently, we are only onboarding MDS. You do not need to register for a HARP/iQIES account for Payroll Based Journal (PBJ) submissions.
Resources
For more information on HARP or iQIES, please refer to the following resources:
HARP
Fact sheet on HARP Identity Proofing FAQs related to HARP
iQIES
iQIES Getting Started Overview iQIES Onboarding Guide iQIES Security Official: Manage Access Job Aid iQIES Quick Reference Guide – Provider Security Official iQIES User Role MatrixResources: Updated PRF Reporting & OIG to Investigate
Updated PRF Reporting Requirements
HRSA published an updated Provider Relief Fund (PRF) Distributions and American Rescue Plan (ARP) Rural Distribution Post-Payment Notice of Reporting Requirements on October 27, 2022. Key updates include reporting guidance for ARP Rural funding recipients and the addition of reporting periods 5, 6 and 7.
OIG to Investigate Skilled Nursing Residents with Potentially Preventable Hospitalizations
The HHS Office of the Inspector General (OIG) recently announced an additional investigation for their 2022 work plan. Previous CMS studies found that five conditions constituted 78 percent of the long-term care resident transfers to hospitals.
The five conditions:
• Pneumonia
• Congestive Heart Failure
• UTIs
• Dehydration
• Chronic Obstructive Pulmonary Disease/Asthma
Additionally, sepsis is often considered a preventable condition. HHS Office of the Inspector General (OIG) will review inpatient hospitalizations of SNF residents with any of the five conditions plus sepsis and determine whether the SNF provided services to residents in accordance with their care plans and professional standards of practice (42 CFR § 483.21 and 42 CFR § 483.25).
Additional Resources: KY Medicaid Renewal Process
KY Medicaid Renewal Process
Public Health Emergency (PHE) is set to expire on January 11, 2023. CMS is required to give a 60-day notice prior to the PHE ending. If the PHE is ending on January 11, 2023, CMS will issue notice by November 12, 2022.
Once the PHE ends, Kentucky Medicaid will begin the “unwinding” process for renewal/recertifications. Please be re-educating and preparing for the renewal/recertification process. The Hargis team is available to assist with a “refresher “ on the renewal process.
If you need assistance, please contact our office. Call us at (270) 726-4033.
UnitedHealthcare: Get ready to submit electronically in 2023

UHC will require electronic claim submissions, claim attachments, and reconsideration and appeal requests as of 1/1/2023
In 2023, network (contracted) health care professionals, practices and facilities will be required to submit claim submissions, claim attachments, and reconsideration and appeal requests to UnitedHealthcare electronically. In response to feedback from members, we’ll also emphasize and encourage the use of digital ID cards for commercial plans.
We recognize that these changes are significant, so we’re alerting you early to give you more time to plan ahead. The effective dates for these incoming paper-to-digital transitions will be announced in Network News at least 90 days prior to the change.
Here’s a preview of what to expect with these changes, as well as more information on digital ID cards for commercial members.
• Goodbye mailroom, hello computer
• You’ll see digital ID cards from members more often
• Help your staff get ready for digital
Click here to view complete details.
If you need assistance, please contact our office. Call us at (270) 726-4033.
Sarah McIntosh, President

iQIES Patient Assessment Minimum Data Set Launch and Provider Security Official Recruitment
iQIES Patient Assessment Minimum Data Set Launch and Provider Security Official Recruitment
The Quality Improvement and Evaluation System (QIES) is being upgraded to make the system more reliable, scalable, secure, and accessible. The enhanced system, referred to as the Internet Quality Improvement and Evaluation System (iQIES), aims to reduce provider burden and enhance the ability for the Centers for Medicare & Medicaid Services (CMS) to better serve our community. CMS is excited to announce that we are preparing to release the iQIES for Minimum Data Set (MDS) submission in early 2023.
To comply with federal security mandates, CMS is initiating new security requirements for access control to the CMS Quality Systems through Remote Identify Proofing (RIDP) via the Healthcare Quality Information System (HCQIS) Access, Roles, and Profile Management system. To gain access to the iQIES system, all users must create an account and establish credentials in the HCQIS Access Roles and Profile (HARP) system, which is a secure identity management portal provided by CMS. To learn more about HARP, click the HARP link below under Resources to review Frequently Asked Questions.
Through HARP, the level of access for iQIES will be similar to the roles in QIES but with the addition of a Provider Security Official (PSO). The individual designated as the PSO must work for the provider and will be responsible for approving or rejecting iQIES user access requests for their respective organizations, including vendors. A user will not be granted access unless a PSO approves the request. The first PSO for your provider will need to be approved by CMS. Once approved, PSOs can approve additional Provider Security Official role requests.
For your organization to receive access to iQIES, your organization must complete the steps below no later than October 28, 2022:
1. Identify at least one individual who will be the Provider Security Official (PSO). Note: At a minimum, at least one PSO needs to be selected, but CMS highly recommends at least two PSOs are designated so there is a higher likelihood that someone will be available to approve/reject iQIES access requests. The PSO must work for the provider and cannot be a vendor.
2. Create an account in the HARP system using your corporate email address* at: https://harp.cms.gov/register. Note: HARP User IDs cannot be adjusted. As such, please refrain from using facility names or any special characters when creating the HARP User ID. *If the facility handles 2 or less providers and does not have a corporate email domain, the PSO may use a personal email address.
3. Access iQIES at: https://iqies.cms.gov/ and log in with your HARP credentials (completed in step 2 above) to request the Provider Security Official role for YOUR specific provider CMS Certification Number (CCN).
4. Once the PSO role request has been submitted AND approved, you will receive notification via email. At this point you will be one of the designated PSOs for your CCN and have the authority to approve/reject subsequent requests for access of various role types to your provider’s CCN.
Resources: HHS Extension, Medicare Credit Balance Reports and more
Reimbursement Alert: HHS Extends Public Health Emergency Through January 12
Health and Human Services (HHS) Secretary Xavier Becerra renewed the declaration that a public health emergency exists. This is effective October 13, 2022, and will continue for 90 days pursuant to federal law.
Reminder: Medicare Credit Balance Reports Due
As a reminder, the Medicare Credit Balance Report for the quarter ending September 30th is due by October 30, 2022. If we do not receive a completed CMS-838 form and/or certification page for an individual provider transaction access number (PTAN) timely, we will suspend all claim payments at 100%.
• Ensure your report is legible and received timely. Don't worry about delivery delays or technical issues with fax transmissions. myCGS allows you to complete and submit the required information electronically and instantly.
• Receive confirmation. myCGS will send a message to your inbox to confirm receipt of the form.
• Check status. Once accepted, myCGS will also send a message with a submission ID you can use to check the status.
Avoid suspension of your Medicare payments! Reference the myCGS User Manual (Financial) for step-by-step instructions and submit your Medicare Credit Balance Report in myCGS today!
Click here for complete details from the CGSmedicare.com website.
KY DMS Encourages Providers to Check Their Revalidation Due Date
Once the Public Health Emergency (PHE) is lifted, Providers with a past due revalidation must be brought back in compliance. KY DMS encourages Providers and Credentialing Agents to complete and submit a revalidation as soon as possible. This will allow KY DMS to review and process revalidations in a timely manner.
Click here for complete details from the chfs.ky.gov website.
MDS Transition from QIES to iQIES

MDS Transition from QIES to iQIES
CMS has announced they are preparing to release the Internet Quality Improvement Evaluation System (iQIES) for MDS submission in early 2023. CMS encourages Providers to assign Provider Security Officials and request access to iQIES as soon as possible. CMS recommends at least two Provider Security Officials (PSO) be designated per provider. The iQIES will consolidate and replace functionality form the QIES, CASPER and ASPEN legacy systems. The PSO will have the responsibility of approving all iQIES users, including vendors that may need access on behalf of the provider.
CMS has released the onboarding schedule and expects to contact providers regarding Security Officials by the end of October and begin general on-boarding communication by mid-November.
Click here to view the onboarding schedule.
Click here to view the iQIES Quick Reference Guides/Job Aids.
Register Today! 2022 Kentucky Fall Road Show
Upcoming Event: Kentucky Fall Roadshow
The CGS Provider Outreach and Education (POE) team is on the road again to Louisville and Erlanger, Kentucky!
Each day’s agenda is the same and includes presentations on topics of interest to both Medicare Part A and Part B providers and staff. Review the agenda and register now to attend one of the KY Medicare Fall Road Show events on November 2, 2022, in Louisville, or November 4, 2022, in Erlanger, from 9:00am to 4:00pm ET.
Click here for details and to register!
Attention: Facilities and Debt Collectors
Reminder from CMS and CFPB
The Consumer Financial Protection Bureau (CFPB) and the Centers for Medicare & Medicaid Services (CMS) remind you of your responsibilities under the Nursing Home Reform Act (NHRA), Fair Debt Collections Practices Act (FDCPA), and Fair Credit Reporting Act (FCRA).
The NHRA prohibits nursing facilities from requesting or requiring that a third party personally guarantee payment to the facility as a condition of a resident’s admission or continued stay in the facility. Contract terms that conflict with the NHRA are unlawful, and alleged debts resulting from such unlawful contract terms are invalid and unenforceable. Some nursing facilities have attempted to evade this prohibition by creating admission contracts that attempt to hold third parties liable for a resident’s debt. When a nursing facility claims that a non-resident is personally financially responsible for a resident’s bill and engages a third-party debt collector to collect the debt, the debt collector may violate the FDCPA by attempting to collect debts that are invalid under the NHRA. They may also violate the FCRA by furnishing information regarding such invalid debts to consumer reporting agencies.
Nursing facilities that violate the NHRA’s requirements may be subject to enforcement action by state agencies and by CMS. Debt collectors who violate the FDCPA and FCRA may be subject to enforcement actions by the CFPB and other federal and state government agencies, as well as to private actions brought by consumers. We urge nursing facilities and their debt collectors to examine their practices to ensure that they comply with the NHRA, FDCPA, and FCRA.
KOG: Kentucky Online Gateway, Changes Effective October 1
KOG: Kentucky Online Gateway MFA Management
Effective October 1, 2022, you will notice changes when logging into KOG, such as:
1. The KOG Log in screen is upgraded.
2. You will be prompted to register for a Multi Factor Authentication (MFA) method, even if you have done so prior to October 1st.
3. Who primary MFA methods are available:
a. OKTA Verify (recommended)
b. Symantec VIP
*Due to the above changes, the security verification process when contacting the Partner Portal Technical Support Staff has changed. Callers should be prepared to provide the following information on all calls effective 10/3/2022:
• KY Medicaid ID
• Name of the Organization or Provider
• National Provider Identifier (NPI)
• Tax ID (either Federal Employee Identification Number or Social Security Number)
Simple Steps for setting up KOG MFA
Fiscal Year (FY) 2023 Skilled Facility Prospective Payment System Final Rule (CMS 1765-F)

Fiscal Year (FY) 2023 Skilled Facility Prospective Payment System Final Rule (CMS 1765-F)
CMS issued the final rule that updates Medicare payment policies and rates for SNFs for FY 2023. Key provisions included:
• A 2.7% increase to base rates.This resulted from a 5.1% update to rates, including a 3.9% SNF market basket increase plus a 1.5% market basket forecast error adjustment less a .3% productivity adjustment, and a negative 2.3% recalibrated parity adjustment.
• CMS finalized the recalibration of the PDPM parity adjustment factor of 4.6%, to be phased-in over a 2-year period; 2.3% in FY 2023 and 2.3% in FY 2024.
• CMS finalized a 5% cap on annual wage index decreases to smooth year-to-year changes in provider's wage index payments.
• PDPM ICD-10 Code Mappings updates
• SNF QRP - a new process measure added, Influenza Vaccination Coverage among Healthcare Personnel, to begin with FY 2024 SNF QRP. SNFs will submit the measure data through the CDC National Healthcare Safety Network with an initial data submission period from October 1, 2022 through March 31, 2023.
• CMS revised the compliance date for certain SNF QRP Requirements, including the Transfer of Health Information measures and certain standardized patient assessment data elements to October 1 ,2023.
• SNF VBP - performance scores have been suppressed one more year. Performance data will be reported publicly but will not affect payment
• SNF VBP - Several new measures will be added beginning with FY 2026.
• Updates to Requirements for Participation for LTC Facilities including updates to the physical environment requirements and changes to the qualification requirements for the director of food and nutrition services. See rule for details.
Click here to see the final rule.
To receive your final FY 2023 Medicare rates contact one of our accountants today. Call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Rhonda Houchens, Director of Operations

CGS “Dark Days, DDE PPTN Recertification Extension, Kentucky Non-Profit Assistance and more
CGS “Dark Days”
To accommodate the anticipated duration to install the October 2022 release, the CWF Host will observe a Gray Day on Thursday, September 29th and Dark Days beginning on Friday, September 30th through Sunday, October 2nd.
Click here for complete details from the CGSmedicare.com website.
DDE PPTN Recertification Extension
DDE and PPTN users are required to recertify on an annual basis. Therefore, CGS has extended the previous deadline to September 1, 2022. DON’T DELAY!!! You must submit your recertification form prior to the deadline.
• Ohio Part A: 1.615.664.5945
• Ohio Part B: 1.615.664.5927
• Home Health & Hospice: 1.615.664.5947
• Kentucky Part A: 1.615.664.5943
• Kentucky Part B: 1.615.664.5917
Kentucky Nonprofit Assistance Fund
The Nonprofit Assistance Fund was created to provide one-time assistance payments to eligible nonprofit organizations that experienced net negative revenue between calendar year 2020 and 2021. This assistance is being made from a $75,000,000 appropriation from the State Fiscal Recovery Fund of the American Rescue Plan Act of 2021. Applications are being accepted August 1, 2022 through October 1, 2022. If you are a nonprofit, please contact our office regarding assistance with the application process.
Click here to view the Eligibility Checklist.
Kentucky Unemployment System Updates
Kentucky Unemployment recently made several updates. All reports must be filed online. Beginning with 2022 tax reports the department will not have the authority or discretion to fix certain issues such as automated excess wage notices of assessment, delinquent report letters, or automated estimates due to no report in database. Automated estimates will become permanent if missing and no response to 20-day notice. If you have questions, contact Melissa Roberts.
Kentucky Disaster Unemployment Assistance
If you have employees who have become unemployed due to the recent flooding disaster they may qualify for assistance. Affected individuals should visit the Kentucky Career Center website, kcc.ky.gov, or call 502-875-0442 to file their initial claim.
Employee Retention Credits (ERC)
Criteria to qualify employers, including tax-exempt organizations, include either:
• The full or partial suspension of the operation of their trade or business during any calendar quarter because of governmental orders limiting commerce, travel or group meetings due to COVID-19, or
• A significant decline in gross receipts.
*Many governmental orders affected the healthcare sector and therefore could qualify your organization to receive the employee retention credits.
Our firm can assist you with determining if you qualify, recommend an ERC specialist for you to work with, and assist you with gathering the necessary payroll data. We will verify all previous COVID funding received such as PPP loans, PRF funding and state COVID funding remain intact and are accurately reported to your ERC specialist.
Want to learn more? Please contact Rhonda or Sarah for more information. Call us at (270) 726-4033.
iQIES
CMS has announced they will begin transitioning SNF/LTC providers from the old QIES system to the new iQIES system. A security official will first need to be set up. The security official will then be able to add users, vendor and third-party users. Security Official set up will start August 15, 2022 with Regions 1 & 2. KY is in Region 4 and is scheduled to begin September 12th. CMS plans to have MDS transmissions in iQIES by early 2023. The timeline, training and onboarding guides should be coming soon on the QTSO site.
NHSN IDs
NHSN and CMS has identified an issue with several providers having an extra organizational ID associated with their CCN. This may have occurred when setting up to submit COVID reporting with NHSN. This could cause a provider to receive out of compliance notices. If NHSN or CMS contacts you regarding this, make sure to address and correct.
Consequences of Severe Storms, Flooding, Landslides, and Mudslides in Kentucky in 2022
Consequences of Severe Storms, Flooding, Landslides, and Mudslides in Kentucky in 2022
Department of Health and Human Services issued this letter regarding the 3-day inpatient hospital stay and additional 100-day benefit for SNF’s with consequences of severe storms, flooding, landslides, and mudslides in Kentucky in 2022.
SNF care without a 3-day inpatient hospital stay will be covered for beneficiaries who experience dislocations or are otherwise affected by the emergency, such as those who are:
• Evacuated from a nursing home in the emergency area,
• Discharged from a hospital (in the emergency or receiving locations) in order to provide care to more seriously ill patients, or
• Need SNF care as a result of the emergency, regardless of whether that individual was in a hospital or nursing home prior to the emergency.
Also, a one-time renewal of 100-day benefit is available. This is only available for beneficiaries who have been delayed or prevented by the emergency itself from commencing or completing the process of ending their current benefit period and renewing their SNF benefits that would have otherwise occurred.
Click here to view the letter from the Department of Health and Human Services.
Nursing Home Five Star Rating Changes

Nursing Home Five Star Rating Changes
With the July 2022 Care Compare refresh, CMS revised the Nursing Home Five Star Quality Rating System to include weekend staffing and staff turnover measures. To emphasize the importance of staffing, CMS will no longer add a star to the overall rating of facilities that have a four-star staffing rating, only those that have a five-star staffing rating will receive the one-star add-on to their overall rating. Visit the links below for more information.
Click here to visit the CMS website for more information. or click one of the direct links below.
• State Survey Agency Directors Memorandum (PDF)
Questions? Call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Rhonda Houchens, Director of Operations

Reminder: Medicare Credit Balance Report
Reminder: Medicare Credit Balance Report
As a reminder, the Medicare Credit Balance Report for the quarter ending June 30, 2022, is due postmarked by July 30, 2022.
A Medicare credit balance is an amount determined to be refundable to the Medicare program for an improper or excess payment made to a provider due to patient billing or claim processing errors. Each provider must submit a quarterly Medicare Credit Balance Report (CMS-838) and certification for each individual PTAN.
Submit your CMS-838/Certification within 30 days of the quarter end date to ensure timely receipt and processing. Use one of the following options. Do not use multiple options or submit duplicate reports.
CGS Information (Check your MAC website if different)

Click here to view the Medicare Credit Balance Report PDF.
Click here for more information.
Please contact our team with questions. Call us at (270) 726-4033.
Notification for Employee Retention Credits
Does your business qualify for the Employee Retention Credits?
Criteria to qualify employers, including tax-exempt organizations, include either:
• The full or partial suspension of the operation of their trade or business during any calendar quarter because of governmental orders limiting commerce, travel or group meetings due to COVID-19, or
• A significant decline in gross receipts.
*Many governmental orders affected the healthcare sector and therefore could qualify your organization to receive the employee retention credits.
Our firm can assist you with determining if you qualify, recommend an ERC specialist for you to work with, and assist you with gathering the necessary payroll data. We will verify all previous COVID funding received such as PPP loans, PRF funding and state COVID funding remain intact and are accurately reported to your ERC specialist.
Want to learn more? Please contact Rhonda or Sarah for more information. Call us at (270) 726-4033.
2022 KY Medicaid Rates

2022 KY Medicaid Rates: Revised 7.1.2022
The Department for Medicaid Services will be increasing the Medicaid rates with the full inflationary rate of 3.1%. This is up from last years increase of 2.5% increase. The capital rate component will receive the RS Means construction cost index of 21.33%. Also, the $29 add-on will remain in the rate until June 2024.
If you would like for our office to calculate your projected 7-1-2022 Medicaid rate, please forward your 4-1-2022 Medicaid rate and your January 2022 thru March 2022 Medicaid case mix to our office. Call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Rhonda Houchens, Director of Operations

PRF Period 3
Reporting Period 3
• Deadline to use PRF funds: 6/30/22
• PRF Reporting Portal Opens: 7/1/22
Recipients who received one or more payments during January 1, 2021 to June 30, 2021 have through June 30, 2022 to use these funds. If payments exceeded $10,000 in the aggregate, the reporting time period begins July 1, 2022 for Period 3 and ends September 30, 2022.
Click here for more information regarding PRF reporting requirements.
If you need assistance with PRF reporting, contact our office for assistance. Call us at (270) 726-4033.
Important Notice from MACS: Internet Explorer to be Retired
WPS and CGS Will No Longer Support Internet Explorer
Microsoft has announced it will be retiring Internet Explorer. Following the announcement, 2 Medicare Administrative Contractors (MACS), confirmed Internet Explorer will no longer be supported by the WPS Government Health Administrators or CGS Medicare website portals.
Beginning August 15, 2022, Internet Explorer will no longer be supported to log into your accounts. If you attempt to log in, you will be blocked. If you are an Internet Explorer user, you must use a different browser before August 15th.
We encourage you to begin using Edge, Chrome, Firefox or Safari to ensure you do not experience any technical issues.
Resources: IRS Increases Milage Rate, Kepro, Kentucky Medicaid and more
IRS Increases Mileage Rate
The IRS announced an increase in the standard mileage rate for the remaining 6 months in 2022. Taxpayers may use the optional standard mileage rates to calculate the deductible costs of operating an automobile for business and certain other purposes.
Click here for details from the IRS.gov website.
Kepro: Medical Record Electronic Submission
Centers for Medicare & Medicaid Services (CMS) regulations require providers to send medical records to Kepro electronically via a Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) approved method. Kepro is the Quality Improvement Organization for Region 4. Kepro will pay providers $3.00 for a complete patient record sent in an electronic format.
Kentucky Medicaid Ancillaries
Reminder: KY Medicaid Prior Authorizations
The Department for Medicaid Services reimburses Kentucky Skilled Nursing Facilities for oxygen therapy, Physical Therapy, Occupational Therapy and Speech Therapy. Prior authorizations for these ancillary services was lifted as of 08/11/2021. Effective 5/1/22, therapy authorizations were reinstated.
To discuss current billing and back billing for these services, please give us a call at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Kentucky Medicaid $270 Add-On is Still in Effect
Many facilities have questioned whether they can currently bill Ky Medicaid for the additional $270 for COVID-19 positive patients. The Medicaid rate add-on of $270 became effective on April 1, 2020 and remains in effect until the Public Health Emergency (PHE) ends. Currently, the PHE is set to expire mid-July 2022. Please see the original Provider letter and FAQ for details regarding the $270 add-on billing procedures.
3-Day Stay Waiver

3-Day Stay Waiver
While the 3-Day waiver is STILL IN EFFECT, Centers for Medicare & Medicaid Services (CMS) has been noticeably silent about whether the waiver will continue to be tied to the public health emergency (PHE).
Do you have questions? Call us at (270) 726-4033.
Kyle Fritsch, Billing Manager

FREE to Kentucky Nursing Homes: The Kentucky Wound Care Excellence Program & Grant Opportunity
FREE to Kentucky Nursing Homes: The Kentucky Wound Care Excellence Program
In July 2021, the Kentucky Office of Inspector General announced that Vohra Wound Physicians Management, LLC has been approved by the Centers for Medicare and Medicaid Services (CMS) to use Civil Money Penalty (CMP) funding to provide 150 scholarships for the Vohra Wound Care Course. The Program is designed specifically for registered nurses (RNs) and licensed practical nurses (LPNs) in certified nursing facilities to improve the care they deliver, raise their level of education, and close the existing knowledge gap in wound care provided across the State of Kentucky.
This opportunity will be offered on a first-come, first-serve basis until all the 150 scholarships are claimed. Nurses completing the course will receive 20 continuing education credits (CEUs). The course includes 11 downloadable learning modules, technical support/customer assistance, and program reporting. The program’s training structure ensures that scholarship recipients will have access to the materials indefinitely as an ever-present guide to sustain lessons learned.
For more information and to register for the program:
• Click here to learn more from VohraWoundCare.com.
• Click here to view the Kentucky Wound Care Excellence Program Information Sheet.
Grant Opportunity for Purchase of Aids to Increase or Improve Air Quality for In-person Visitations
As of February 2, 2022, certified nursing facilities may apply for up to an additional $3,000 of Civil Money Penalty (CMP) Nursing Home Visitation Aid Grant funds for the purchase of indoor portable fans and/or indoor portable air cleaners with high-efficiency particulate air (HEPA, H-13 or -14) filters, to increase or improve air quality to aid in-person visitation for residents. Expenses incurred on or after the release of Memorandum QSO-20-39-NH FAQ Revised, February 2, 2022, are eligible for reimbursement.
CMP Nursing Home Visitation Aid Grant funds are still available for the purchase of tents or other shelter for outdoor visitation and/or clear dividers, installation, installation materials and shipping costs for in-person visitation aids. All eligible expenses incurred on or after September 17, 2020, are eligible for reimbursements, up to a maximum of $3,000.
For more information and to apply for CMP Nursing Home Visitation Aid Grant funds:
• CMP Application for In-Person Visitation Aid Requests FAQ
• Application Form for Visitation Aid Project
Click here to send an email to Lena Mullins-Datko, CMP Grant Administrator: lena.mullinsdatko@ky.gov.
Make Your Voice Heard: Let CMS Know You Oppose Medicare Payment Cuts
Make Your Voice Heard: Let CMS Know You Oppose Medicare Payment Cuts
The proposed rule provides for a net market basket increase for SNFs of 3.9% beginning October 1, 2022, but a proposed parity adjustment of 4.6%. CMS estimates a net decrease Medicare SNF payment would be approximately $320 million in FY 2023.
Now is the time to make your voice heard and tell CMS Administrator Chiquita Brooks-LaSure just how devastating lower Medicare reimbursement rates will be, particularly as nursing homes are still dealing with increased expenditures due to the pandemic, low census, and the ongoing staffing crisis.
DDE Recertification Extended Deadline
Attention CGS J15 Providers!
CGS J15 planned to conclude the Annual Recertification process on April 30, 2022. Currently, we have over 3000 users who have not completed the annual recertification.
In an effort to ensure that DDE/PPTN access is not terminated for these users, CGS has decided to extend the Annual DDE PPTN Recertification period to May 31, 2022. If you have users that need to complete the Annual Recertification, please complete the following form as soon as possible:
Click here to view the Annual DDE PPTN Recertification Form.
Don’t Delay! Once the termination process has begun for a user, a J15 DDE PPTN Application/Reactivation form must be submitted. The normal 20 business days for processing will be applied to the new application. Please resubmit your Annual Recertification form to prevent any termination or access to DDE/PPTN.
CMS Recent Announcement Regarding PHE and Related Waivers

CMS Recent Announcement Regarding PHE and Related Waivers
Public Health Emergency (PHE) Extended
On April 12, the U.S. Department of Health and Human Services (HHS) announced the extension of the public health emergency (PHE). The extension is for 90 days.
Click here for more information.
The PHE extension also extends the three-day stay and telehealth waivers for the additional 90 days.
However, CMS’ release of QSO-22-15 stands as published on April 7, 2022.
CMS to End Specific Blanket Waivers
The Centers for Medicare & Medicaid Services (CMS) announced guidance to restore certain minimum standards for compliance. This is being done by phasing out some temporary emergency declaration waivers that have been in effect throughout the COVID-19 PHE.
On April 7, 2022, CMS issued this press release.
The memorandum details the specific waivers that will end 30 days and 60 days from issuance.
Click here to view the memorandum.
If you need assistance, please contact our office. Call us at (270) 726-4033.
Sarah McIntosh, President

Resources: PHE Declarations, Blanket Waivers, and New Proposed Rule
Public Health Emergency Declarations
The Public Health Emergency was set to end on April 15, 2022. The latest HHS extension for the Public Health Emergency is effective April 16, 2022 through July 15, 2022.
Click here to view complete details from the U.S. Department of Health & Human Services.
CMS to End Specific Blanket Waivers
The Centers for Medicare & Medicaid Services (CMS) announced guidance to restore certain minimum standards for compliance. This is being done by phasing out some temporary emergency declaration waivers that have been in effect throughout the COVID-19 PHE.
Click here to view the press release from CMS.
The memorandum from CMS details the specific waivers that will end 30 days and 60 days from issuance.
Click here to view the memorandum details.
Fiscal Year (FY) 2023 Skilled Nursing Facility Prospective Payment System Proposed Rule (CMS 1765-P)
On April 11, 2022, the Centers for Medicare & Medicaid Services (CMS) issued a proposed rule that would update Medicare payment policies and rates for skilled nursing facilities under the Skilled Nursing Facility Prospective Payment System (SNF PPS) for fiscal year (FY) 2023.
Medicaid Ancillary PAs: Due May 1, 2022

Medicaid Ancillary PAs: Due May 1, 2022
In the last issue of KAHCF Connections, the association announced that effective May 1, 2022, all FFS and MCOs may require a Prior Authorization (PA) for Skilled Nursing Facility providers. The association issued the announcement after receiving a Provider Letter notice dated March 16, 2022. (See link below.)
In a Billing Work Group meeting this morning, Carewise Peer Review Organization (PRO) representative Tracy Treat provided information to the Work Group that will help in the transition. Effective May 1, 2022, nursing facilities will again be required to obtain a PA for ancillary services, and to assist facilities with this activity, the PRO will follow the steps below to ensure a smooth transition:
For residents receiving Physical, Occupational, and Speech Therapy, please follow the steps below:
• Therapy plan of care that begins prior to but spans May 1st, submit the following documents to obtain Prior Authorization for your plan of care dates
• Therapy plan of care begins May 1st
For residents needing Oxygen authorizations, the following outlines the process to be followed:
• Please complete the spreadsheet (link below) for any resident in your facility that is receiving oxygen and email back to PRO at the following email address: Ronda.Phillips@Carewisehealth.com
• Facilities will be required to submit all requests via fax once the spreadsheet has been submitted back to PRO
Should providers have any questions regarding the process mentioned above, please email Tracy Treat at tracyjo.treat@carewisehealth.com or call Carewise at (800) 292-2392.
Click here to view the Provider Letter notice dated March 16, 2022.
Click here to view the Oxygen Authorization Spreadsheet.
If you need assistance, please contact our office. Call us at (270) 726-4033.
Sarah McIntosh, President

Medicare FFS Claims: 2% Payment Adjustment (Sequestration) Changes

Medicare FFS Claims: 2% Payment Adjustment (Sequestration) Changes
The Protecting Medicare and American Farmers from Sequester Cuts Act impacts payments for all Medicare Fee-for-Service (FFS) claims:
• No payment adjustment through March 31, 2022
• 1% payment adjustment April 1 – June 30, 2022
• 2% payment adjustment beginning July 1, 2022
Click here to visit the CMS website for more information.
If you need assistance, please contact our office. Call us at (270) 726-4033.
Leah Shoulders, Billing Manager

Important Notice: New Procedures in Place to Protect from Fraudulent Direct Deposit Requests
Important Notice: New Procedures in Place to Protect from Fraudulent Direct Deposit Requests
We would like all payroll processors to send the signed Authorization forms for direct deposits with any banking changes for your employees.
Although there is no cure-all to prevent fraud in your business, we would like to help you by instituting some fraud prevention strategies.
We receive warnings from our bank monthly to watch out for fraud.
One example: the employer receives an email from the employee directing them to change their direct deposit to a different account, most often a pay card. The defrauder has hacked the employee email and directed the employer to give them the funds, which they draw out of the fraudulent account on pay day. The bank says this type of fraud is so rampant and so hard to trace.
The bank recommends that you do not accept banking changes from employees through email. We would like to encourage that you personally talk to any employee that needs to make a bank change and have them fill out the Authorization form. (Please contact us if you need an updated form.)
We would also like to be able to track any payroll changes more easily. So if you have banking changes, please send them with entire payroll info on payroll processing day. This would be helpful in letting us know that you are aware of all banking changes being made for your employees.
If you are a client that puts in your own employee information, we strongly suggest that you also have each employee fill out the Authorization form, and do not accept emailed changes to banking info.
Thank you and please let us know if you have any questions.
If you have any questions, please contact Veronica, our payroll partner with Abacus. veronica@abacuspaysystems.com
Veronica Ramsey, Manager of Abacus PaySystems

Resources: Medicaid Prior Authorization Guidance, Quarterly Reports and more
Medicaid Prior Authorization Guidance
The Department for Medicaid Services (DMS) is reinstating the therapy PA’s effective May 1, 2022.
Click here to view the letter from DMS.
March 2022 Interim Quarterly Confidential Feedback Reports
The March 2022 Interim Quarterly Confidential Feedback Reports for the fiscal year (FY) 2023 Skilled Nursing Facility Value-Based Purchasing (SNF VBP) Program are now available to download via the Quality Improvement and Evaluation System (QIES)/Certification and Survey Provider Enhanced Reports (CASPER) reporting system. These reports contain interim stay-level data for the SNF 30-Day All-Cause Readmission Measure (SNFRM) for 10/1/2020-6/30/2021 (Quarter 1-Quarter 3 of the FY 2023 SNF VBP Program performance period, FY 2021). The interim data contained in these reports are not final and are subject to change, and thus are not eligible for the SNF VBP Program's Review and Correction process.
The March 2022 reports contain stay-level data protected by the Health Insurance Portability and Accountability Act of 1996 (HIPAA). Any disclosure of protected health information (PHI) should only be in accordance with, and to the extent permitted by, the HIPAA Privacy and Security Rules and applicable law. When referring to the contents of the report, use the Line Number (located in the leftmost column of the '2 - Eligible Stays' tab) of the stay in question.
For questions about accessing your SNF's report, which can only be accessed via CASPER, please contact the QIES Technical Support Office Help Desk at iqies@cms.hhs.gov
Click here for more information about the SNF VBP Program from the CMS website.
If you have any additional questions, please contact the SNF VBP Program Help Desk by emailing: SNFVBP@rti.org
Biden’s Planned Nursing Home Reform: FACT SHEET: Protecting Seniors by Improving Safety and Quality of Care in the Nation’s Nursing Homes
All people deserve to be treated with dignity and respect and to have access to quality medical care. The President is committed to ensuring that all Americans, including older Americans and people with disabilities, live in a society that is accessible, inclusive, and equitable. To accomplish that goal, the Administration continues to be committed to home- and community-based services and ensuring that in no case should a health care facility be causing a patient harm. The President believes we must improve the quality of our nursing homes so that seniors, people with disabilities, and others living in nursing homes get the reliable, high-quality care they deserve. That’s why he is announcing a set of reforms—developed by and implemented through the Department of Health and Human Services (HHS)—that will improve the safety and quality of nursing home care, hold nursing homes accountable for the care they provide, and make the quality of care and facility ownership more transparent so that potential residents and their loved ones can make informed decisions about care.
To do this, the reforms the President is announcing will ensure that:
• Every nursing home provides a sufficient number of staff who are adequately trained to provide high-quality care;
• Poorly performing nursing homes are held accountable for improper and unsafe care and immediately improve their services or are cut off from taxpayer dollars; and
• The public has better information about nursing home conditions so that they can find the best available options.
Click here for more information from the White House.
Common Working File (CWF) will observe Dark Days in April 2022
To accommodate the anticipated duration to install the April 2022 release, the CWF Host will observe Dark Days beginning on Friday, April 1, 2022, through Sunday, April 3, 2022.
What this means to you:
• It is customary for contractors to hold claims for several days following a quarterly release. Claims that are submitted prior to the release that would have been processed through the CWF during this period will be held until the nightly system cycle on Monday, April 4, 2022.
• We anticipate claims will still be processed within a normal timeframe and these slight delays will not affect the timeliness of your payments.
• This will not affect your ability to access beneficiary eligibility information through myCGS or the IVR, but the information will not update during the dark day period.
Note for Home Health and Hospice Providers: Notices of Admission (NOAs) and Notices of Election (NOEs) can still be submitted to CGS during this period. If you feel that a late submission of an NOA/NOE was caused by the dark day, appropriate documentation must be submitted.
Click here for more information from the CGS Medicare website.
NEW Grant Opportunity, Per the Office of Inspector General: Revised 3/10/22
Per the Office of Inspector General February 2002 newsletter, there is a NEW grant opportunity for purchase of aids to increase or improve air quality for in-person visitations. Certified nursing facilities may apply for up to an additional $3,000 of Civil Money Penalty (CMP) Nursing Home Visitation Aid Grant funds for the purchase of indoor portable fans and/or indoor portable air cleaners with high-efficiency particulate air (HEPA, H-13 or -14) filters, to increase or improve air quality to aid in-person visitation for residents. Expenses incurred on or after the release of Memorandum QSO-20-39-NH FAQ Revised, February 2, 2022, are eligible for reimbursement.
For more information and to apply for CMP Nursing Home Visitation Aid Grant funds:
1. CMP Application for In-Person Visitation Aid Requests FAQ
2. Application Form for Visitation Aid Project
Contact Lena Mullins-Datko, CMP Grant Administrator with questions of the COVID-19 Visitation Aid Grant Funds.lena.mullinsdatko@ky.gov
HRSA Reporting Period 2 submissions are due by March 31, 2022

HRSA Reporting Period 2 submissions are due by March 31, 2022
Providers who received one or more General and/or Targeted PRF payments exceeding $10,000, in the aggregate, from July 1, 2020 to December 31, 2020 must report on their use of funds in Reporting Period 2. The deadline to use funds for Period 2 was December 31, 2021. For most Nursing Facilities these payments received were the Nursing Home Infection Control Distribution and the Quality Incentive Payments received in 2020. The terms and conditions for these funds were different than the general distributions reported on in Period 1.
Click here to visit the HRSA website for more information regarding Period 2 requirements.
If you need assistance with PRF reporting or determining which expenditures meet these terms and conditions, contact our office for assistance. Call us at (270) 726-4033.
Rhonda Houchens, Director of Operations

HRSA Continues Phase 4 Funding Release and KY Disaster Relief Sales and Use Tax Refund
HRSA Continues Phase 4 Funding Release
Phase 4 General Distribution payments began in December 2021. Payments were released in December and January. HRSA was still working through some provider’s applications this month and indicated if you had not received a No Pay Letter, a Phase 4 award was forthcoming. Once all Phase 4 awards are made, payment breakouts should become available.
Click here to visit the HRSA website for more information regarding Phase 4 funding.
KY Disaster Relief Sales and Use Tax Refund
This federal disaster declaration activates the provisions of KRS 139.519, which provides for a refund of Kentucky sales and use tax paid for building materials permanently installed in the repair or replacement of structures damaged in counties covered under a federal disaster relief declaration.
This state assistance was initially available to property owners in Breathitt, Clay, Estill, Floyd, Johnson, Lee, Magoffin, Martin, and Powell counties.
The additional counties now eligible for individual assistance are Anderson, Boyd, Clark, Fayette, Franklin, Greenup, Jackson, Jessamine, Knott, Laurel, Lawrence, Leslie, Letcher, Lincoln, Madison, Morgan, Owsley, Perry, Pulaski, Rockcastle, Warren, and Woodford.
Refunds apply to purchases made on or after the date of the disaster declaration for individual relief. Applicants have three years from the date the area is declared a federal disaster to submit their refund claims to the Kentucky Department of Revenue.
Click here to view frequently asked questions.
Medicaid $270 Add-On Still in Effect

Medicaid $270 Add-On Still in Effect
Kentucky Medicaid $270 add-on is still in effect: Many facilities have questioned whether they can currently bill Ky Medicaid for the additional $270 for COVID-19 positive patients. The Medicaid rate add-on of $270 became effective on April 1, 2020 and remains in effect until the Public Health Emergency (PHE) ends. Effective January 16, 2022, the Public Health Emergency was renewed. The U.S. Department of Health and Human Services (HHS) extends the PHE in 90 day increments.
Click here for details of the renewal from the HHS.gov website.
Do you have questions? Call us at (270) 726-4033.
Kyle Fritsch, Billing Manager

Tax Season to Begin January 24, 2022
Tax Season to start on Jan. 24
The Internal Revenue Service will begin processing and accepting 2021 tax returns on Monday, Jan. 24, and the filing deadline will be Monday, April 18. The IRS expects that most taxpayers will receive their refund within 21 days of when they file electronically, unless there’s an issue with processing their tax return.
Resources: Kentucky Medicaid Bed Reservation, Single Audit, Annual DDE PPTN Recertification and Public Health Emergency Renewed
Kentucky Medicaid Bed Reservation
Effective April 1, 2020 Department for Medicaid Services increased the bed reservation days to 30 per calendar year through the end of the Public Health Emergency. Therefore, Kentucky Medicaid patients have 30 bed reservation days as of 1/1/2022.
Single Audit
Recipients that spend a total of $750,000 or more in federal funds, including Provider Relief Fund (PRF) payments and other federal financial assistance, during their fiscal year are subject to Single Audit requirements, as set forth in the regulations at 45 Code of Federal Regulations (CFR) § 75 Subpart F.
Please reach out to our office to see if your facility is subject to Single Audit requirements. Call us at (270) 726-4033 or email us at: accountants@hargisandassociates.com
Annual DDE PPTN Recertification
DDE and PPTN users are required to recertify on an annual basis. To ensure a smooth transition for the 2022 DDE PPTN Recertification, CGS has added a user-friendly PDF form: Annual DDE PPTN Recertification Form.
• Deadline: Part A deadline is March 31, 2022
• FAX Completed form to: Kentucky Part A: 1.615.664.5943
Public Health Emergency Renewed
As a result of the continued consequences of the Coronavirus Disease 2019 (COVID-19) pandemic, on this date and after consultation with public health officials as necessary, I, Xavier Becerra, Secretary of Health and Human Services, pursuant to the authority vested in me under section 319 of the Public Health Service Act, do hereby renew, effective January 16, 2022, the January 31, 2020, determination by former Secretary Alex M. Azar II, that he previously renewed on April 21, 2020, July 23, 2020, October 2, 2020, and January 7, 2021, and that I renewed on April 15, 2021, July 20, 2021, and October 18, 2021 that a public health emergency exists and has existed since January 27, 2020, nationwide.
Click here for details from the HHS.gov website.
CMS To Post Nursing Home Weekend Staffing, Staff Turnover Data
CMS To Post Nursing Home Weekend Staffing, Staff Turnover Data
It’s a good time to review your staff turnover and weekend staffing levels as CMS announces new guidance effective immediately. Skilled Nursing News: CMS To Post Nursing Home Weekend Staffing, Staff Turnover Data CMS Notice: QSO-22-08-NH, Nursing Home Staff Turnover and Weekend Staffing Levels
Resources: Phase 4 Payments and Sequestration Medicare FFS Claims
Phase 4 Payments
On December 16, The Department of Health and Human Services (HHS) sent notifications to facilities regarding Phase 4 payments. The Phase 4 payments included a base payment and/or bonus payment. The Base payments were calculated as a percentage of expenses and revenues reported in your application for the period from July 1, 2020 to March 31, 2021. Bonus payment were calculated based on Medicare, Medicaid and CHIP administrative claims data from January 1, 2019 through September 30, 2020.
More detailed information on payment methodology is available here.
Medicare FFS Claims: 2% Payment Adjustment (Sequestration) Changes
CMS posted the below information in their December 16th MLN Connects. The Protecting Medicare and American Farmers from Sequester Cuts Act impacts payments for all Medicare Fee-for-Service (FFS) claims:
• No payment adjustment through March 31, 2022
• Contact information for one or two individuals from your organization to support administration and oversight of your account
• 1% payment adjustment April 1 – June 30, 2022
• 2% payment adjustment beginning July 1, 2022
ARP Rural Payment

ARP Rural Payment
On November 23, 2021 HRSA began distributing ARP Rural payments. The payments were based on the amount and type of Medicare and Medicaid services provided to rural beneficiaries from January 1, 2019 thru September 30, 2020.
Approximately 96 percent of ARP Rural applications have now been processed. Providers who have not yet received any communication regarding their payment determination will be notified as soon as HRSA completes the review and processing of the remaining applications.
Click here to access the public dataset of payment names.
The automated payments were sent via Optum Bank. If your facility is listed on the dataset and has not received the payment you will need to sign up for an Optum Pay account.
You will need to have the following information available to complete the Optum Pay account.
• Contact information (name, phone number and email address)
• Contact information for one or two individuals from your organization to support administration and oversight of your account
• Your organization’s banking information (routing number, account number and account type)
• Voided check or bank letter
• IRS Form W-9
Blog by Sarah McIntosh, Director of Operations

Reduced Payment Effective 1-1-2022
Reduced Payment Effective 1-1-2022
Effective January 1, 2022, there will be reduced payment for physical and occupational therapy services provided by PTAs or OTAs. Modifiers CQ and CO will be required on claims for PTA and OTA services.
FY 2023 SNF VBP Program December 2021 Quarterly Reports Now Available
FY 2023 SNF VBP Program December 2021 Quarterly Reports Now Available
The December 2021 Quarterly Confidential Feedback Reports for the fiscal year (FY) 2023 Skilled Nursing Facility Value-Based Purchasing (SNF VBP) Program are now available to download via the Quality Improvement and Evaluation System (QIES)/Certification and Survey Provider Enhanced Reports (CASPER) reporting system. These reports contain facility and stay-level data and results for the SNF 30-Day All-Cause Readmission Measure (SNFRM) for FY 2019, the FY 2023 SNF VBP Program baseline period. These results will be used for the FY 2023 SNF VBP scoring and incentive payment multiplier calculations that will take effect October 1, 2022.
SNFs can review and submit corrections to their FY 2019 readmission rate calculations only up to 30 days following this report being made available, until January 1, 2022. Correction requests should be emailed to SNFVBP@rti.org with the subject line ‘SNF VBP Review and Correction Inquiry’ along with your SNF’s CMS Certification Number (CCN), your SNF’s name, the correction request, and the reason for requesting the correction.
The December 2021 reports contain stay-level data protected by the Health Insurance Portability and Accountability Act of 1996 (HIPAA). Any disclosure of protected health information (PHI) should only be in accordance with, and to the extent permitted by, the HIPAA Privacy and Security Rules and applicable law.
When referring to the contents of the report, use the Line Number (located in the leftmost column of the ‘2 - Eligible Stays’ tab) of the stay in question.
For questions about accessing your SNF’s report, please contact the QIES Technical Support Office Help Desk at iQIES@cms.hhs.gov.
Click here for more information about the SNF VBP Program.
If you have any additional questions, please contact the SNF VBP Program Help Desk at SNFVBP@rti.org.
Sincerely, the SNF VBP Team
HRSA Sent Emails by Error

It was brought to our attention that Health Resources & Services Administration (HRSA) sent emails in error stating that individual providers would be ineligible for Phase 4 because Reporting Period 1 applications had not been filed. If your facility receives an email stating this, we recommend that you contact HRSA Provider Support at 1-866-569-3522.
Also, facilities started receiving Rural distribution payments on 11/23/21. The Phase 4 distributions will be paid in December.
Click here for more details on this.
Do you have questions? Call us at (270) 726-4033.
Melodie G Bingham, CPA, Sr. Accountant

Medicare Part A & B and Deductibles
CMS has released the 2022 premiums, deductibles, and coinsurance amounts for the Medicare Part A and Part B programs, and the 2022 Medicare Part D income-related monthly adjustment amounts.
Medicare B premiums
$170.10 for 2022 The increase in the standard monthly premium—from $148.50 in 2021 to $170.10 in 2022
Medicare B deductible
$233 for 2022 The annual deductible for Medicare Part B beneficiaries is increasing from $203 in 2021 to $233 in 2022.
Medicare A coinsurance
$194.50 for 2022 For beneficiaries in skilled nursing facilities, the daily coinsurance for days 21 through 100 of extended care services in a benefit period will be $194.50 in 2022 ($185.50 in 2021).
Medicare Open Enrollment
Medicare Open Enrollment for 2022 began on October 15, 2021, and ends on December 7, 2021.
During this time, people eligible for Medicare can compare 2022 coverage options between Original Medicare, and Medicare Advantage, and Part D prescription drug plans.
Humana Update
Humana
It has been brought to our attention that Humana has mailed Post-Pay Medical Record Request and Pre-Pay Medical Record Request in ERROR. Humana should be mailing cancelation letters soon. If your facility receives a Post-Pay Medical Record Request or Pre-Pay Medical Record Request for ANY claim that naviHealth manages, please forward to Sarah McIntosh at: smcintosh@hargisandassociates.com
Apply Now for Phase 4 and ARP Rural Distributions

Provider Relief Fund Phase 4 and American Rescue Plan (ARP) Rural payments application
The application will close on October 26, 2021 at 11:59 p.m. ET. Applications must undergo a number of validation checks before financial information is submitted so providers are encouraged to begin their application as soon as possible to ensure they are able to meet the deadline. Information on the documents and information needed to apply can be found in the resources following.
In order to streamline the application process and minimize administrative burdens, providers will apply for both programs in a single application, and HRSA will use existing Medicaid, Children's Health Insurance Program (CHIP), and Medicare claims data in calculating portions of these payments.
For all the details regarding this application and payments visit www.hrsa.gov/provider-relief/future-payments.
If you need assistance completing your application contact one of our client managers today at (270) 726-4033.
Blog by Sarah McIntosh, Director of Operations

Flu Vaccine Amounts have been published for 2021-2022 Season
Flu Vaccine Amounts have been published for 2021-2022 Season
For SNF’s, Medicare B pays for patients that receive the influenza, pneumococcal and Hepatitis B vaccines. As a reminder, the vaccines are a separate Part B inpatient benefit when rendered to beneficiaries in a covered Part A stay. Therefore, the SNF can be reimbursed for the vaccines given to all patients that have Medicare B, regardless if the patient is using Medicare A benefits or not. Reference the Medicare Claims Processing Manual, Chapter 6, Section 20.4 for details.
Click here to visit the CMS.gov website.

Resources: PRF Reporting Period 2 and KY Medicaid Prior Authorizations
PRF Reporting Period 2
It’s not too early to plan for the next reporting cycle. Period 2 funds received between July 1, 2020 to December 31, 2020 must be used by December 31, 2021. Visit HRSA’s website for details and contact our office to discuss allowable expenses and details for Period 2 Funds.
Click here to visit the HRSA's website.
KY Medicaid Prior Authorizations
Prior authorization for Nursing Facility (PT12), ancillary services is lifted, effective for dates of service 08/11/2021 until further notice. This decision is to assist with lifting administrative burdens associated with an influx of COVID patients.
New Provider Relief Funding Available

The Department of Health and Human Services (HHS) announced Friday September 10th, $25.5 billion in new funding for health care providers affected by COVID-19 pandemic will be available.
Phase 4 General Distribution - $17 billion will be available to a broad range of providers who can document revenue loss and expenses associated with the pandemic.
American Rescue Plan (ARP) Rural - $8.5 billion will be available to providers who serve Medicaid/CHIP and Medicare beneficiaries living in Federal Office of Rural Health Policy (FORHP)-defined rural areas.
Phase 3 Reconsiderations – The methodology utilized to calculate Phase 3 payments is now available and an opportunity to request a reconsideration. Further details of the reconsideration process are forthcoming.
Grace Period for Reporting Period 1- HHS has announced a 60-day grace period to help providers struggling to meet the deadline of September 30, 2021 for Period 1 PRF Reporting. The deadlines to use the funds and the reporting time period did not change. HHS will not initiate collection activities or similar enforcements for noncompliant providers during the grace period.
Click here for more details on this.
Do you have questions? Call us at (270) 726-4033.
Rhonda Houchens, Director of Operations

Resources: Vaccine Mandate, CMS Updates, KY General Assembly Session Bills Passed and more
President Biden Announces New Vaccine Mandate- On September 9, 2021
President Biden announced new vaccine requirements including requiring vaccinations for nursing home workers, hospitals, dialysis facilities, ambulatory surgical settings, home health agencies and others as a condition to participate in Medicare and Medicaid programs. CMS is developing an Interim final Rule with Comment Period that will be issued in October. The compliance deadline is unknown but excepted to be by the end of 2021.
Read the full CMS release here.
In addition to the CMS mandate for vaccinations of Medicare and Medicaid health care providers, the U.S. Department of Labor will issue requirement for employers with over 100 employees to have vaccine mandates and/or testing. Also, all federal employees and contractors will need to be vaccinated.
CMS Updates Medicare COVID-19 Billing Guidance
On September 8, 2021 the Centers for Medicare and Medicaid Services (CMS) updated MLN Matters SE2011. Please take note in this guidance CMS DID NOT change the longstanding blanket 3-day qualifying stay or spell of illness waivers for beneficiary eligibility for SNF Part A coverage.
Click here to view the MLN Matters SE2011.
Reference Waiver guidance is available here.
Proposal to Increase Tax Revenue Through Financial Information
Banks having been notifying their customers of a Biden administration proposal released to increase tax revenue through a more comprehensive collection of financial information on banking customers. If approved financial institutions would be required to report all financial information on accounts with inflow/outflows or balances above $600. Banking institutions are deeply opposed to this proposed legislation. They are concerned about their customers privacy as well as the burden of expense this would place on banks to comply which would ultimately cost their customers. Banks are encouraging their customers to contact their legislators and ask them to oppose this legislation. For more information we encourage you to contact your banking institution.
KY General Assembly Session Bills Passed
As a result of last week’s special session 3 bills were passed including: HJR1, which extended the state or emergency and other special rules until January 15, 2022, SB2, allowing Personal Care Aides to transition to state-registered nurse aides to aide the workforce shortage as well as other provisions and SB3, which appropriates $69 million of American Rescue Plan Act funds to be used for health care, long-term care, and school system COVID-19 testing and management of monoclonal antibody treatment.
Medicaid Add-On Attestation Statement
Medicaid Add-On Attestation Statement
On August 20, 2021, Myers & Stauffer’s help desk emailed providers regarding the attestation of the $29 Medicaid rate add-on. Each nursing facility should return the signed form to Myers & Stauffer by September 30, 2021.
Click here for the Attestation Form.
Hospice & $29 Rate Add-On
Hospice and $29 Rate Add-On
Hospice providers have been approved to receive the $29 Medicaid add-on. If you have not received the $29 Add-on, check with your hospice provider to see when the mass adjustment will be received.
FY 2022 SNF Final Rule Released

FY 2022 SNF Final Rule Released
The Fiscal Year (FY) 2022 Skilled Nursing Facility (SNF) Prospective Payment System (PPS) Final Rule (CMS-1746-F) was released July 29, 2021. Key updates in the rule includes a net 1.2 percent market basket increase, updates to PDPM ICD-10 Code Mappings, SNF QRP additional measures, and SNF VBP changes to FY 2022 and future expansion.
Click here to visit www.CMS.gov for a full overview.
To receive a copy of PDPM rates effective October 1, 2021, please verify your FY 2022 VBP multiplier of .9920 or 1.0 if low volume and contact one of our client managers today.
Blog by Rhonda Houchens, Director of Operations

CY 2022 Medicare B Therapy
CY 2022 Medicare B Therapy
CMS is proposing implementation of the final part of section 53107 of the Bipartisan Budget Act of 2018. Implementation would require CMS, through the use of modifiers (CQ and CO), to identify and make payment at 85% of the otherwise applicable Part B payment amount for physical therapy and occupational therapy services furnished in whole or in part by physical therapist assistants (PTAs) and occupational therapy assistants (OTAs), for dates of service on and after January 1, 2022. Currently, Part B provider are using modifiers CQ and CO for data collection purposes only.
Remember, these changes are for Part B therapy only. CMS will accept comments on the proposed rule until September 13, 2021, and will respond to comments in a final rule.
Resources: ABN Form Renewal and Electronic Plan of Correction (ePOC)
ABN Form Renewal
The Office of Management and Budget approved the Advance Beneficiary Notice of Noncoverage, (ABN). See form CMS-R-131 and link to instructions below for renewal. You must use the renewed form with the expiration date of June 30, 2023, beginning August 31. There are no other changes to the form.
Click here for Form CMS-R-131 (ZIP).
Click here for renewal instructions (PDF).
Click here to visit the CMS ABN Webpage.
Electronic Plan of Correction (ePOC)
Office of Inspector General is encouraging Skilled Nursing Facilities to sign up and begin utilizing Electronic Plan of Correction (ePOC). The plan is to convert everyone over to the ePOC system by January 1, 2022.
Click here for details from www.chfs.ky.gov.
NEW Billing Consultant Packages: Medicare Replacement Insurance

NEW Billing Consultant Packages: Medicare Replacement
Have you considered contracts with Medicare Replacement plans in order to add to your census? We recently helped a facility increase admissions by getting contracts with multiple Medicare Replacement insurances.
Introducing our NEW Billing Consultant Packages...
We offer packages that are made to fit your facility's individual needs. So, whether you need just a little bit of help and guidance to get back on track or someone to step in to take it over, we have a package for you!
Do you have questions? Call us with your questions at (270) 726-4033.
Blog by Leah Shoulders, Billing Manager

Important Changes to the Child Tax Credit
Important changes to the child tax credit; Please contact our office
Recently, there were changes made to the child tax credit that will benefit many taxpayers. As part of the American Rescue Plan Act that was enacted in March 2021, the child tax credit:
• Amount has increased for certain taxpayers
• Is fully refundable (meaning you can receive it even if you don’t owe the IRS)
• May be partially received in monthly payments
The new law also raised the age of qualifying children to 17 from 16, meaning some families will be able to take advantage of the credit longer. The IRS will pay half the credit in the form of advance monthly payments beginning July 15. Taxpayers will then claim the other half when they file their 2021 income tax return. Though these tax changes are temporary and only apply to the 2021 tax year, they may present important cashflow and financial planning opportunities today. It is also important to note that the monthly advance of the child tax credit is a significant change. The credit is normally part of your income tax return and would reduce your tax liability. The choice to have the child tax credit advanced will affect your refund or amount due when you file your return. To avoid any surprises, please contact our office.
Qualifications and how much to expect:
The child tax credit and advance payments are based on several factors, including the age of your children and your income.
• The credit for children ages five and younger is up to $3,600 –– with up to $300 received in monthly payments.
• The credit for children ages six to 17 is up to $3,000 –– with up to $250 received in monthly payments.
To qualify for the child tax credit monthly payments, you (and your spouse if you file a joint tax return) must have:
• Filed a 2019 or 2020 tax return and claimed the child tax credit or given the IRS your information using the non-filer tool
• A main home in the U.S. for more than half the year or file a joint return with a spouse who has a main home in the U.S. for more than half the year
• A qualifying child who is under age 18 at the end of 2021 and who has a valid Social Security number
• Income less than certain limits
You can take full advantage of the credit if your income (specifically, your modified adjusted gross income) is less than $75,000 for single filers, $150,000 for married filing jointly filers and $112,500 for head of household filers. The credit begins to phase out above those thresholds.
Higher-income families (e.g., married filing jointly couples with $400,000 or less in income or other filers with $200,000 or less in income) will generally get the same credit as prior law (generally $2,000 per qualifying child) but may also choose to receive monthly payments. Taxpayers generally won’t need to do anything to receive any advance payments as the IRS will use the information it has on file to start issuing the payments.
IRS’s child tax credit update portal
Using the IRS’s child tax credit and update portal, taxpayers can update their information to reflect any new information that might impact their child tax credit amount, such as filing status or number of children. Parents may also use the online portal to elect out of the advance payments or check on the status of payments.
The IRS also has a non-filer portal to use for certain situations. With any tax law change, it’s important to revisit your full financial roadmap. We can help you determine how much credit you may be entitled to and whether advance payments are appropriate.
Please contact our office today at 270.726.4033 to discuss your specific situation. As always, planning ahead can help you maximize your family’s financial situation and position you for greater success.
Sincerely,
Hargis and Associates LLC
Resources: Provider Relief Reporting & CMS Updates
Provider Relief Fund (PRF) Reporting
The PRF Portal is now open. Reporting Period 1 data is to be reported between July 1 and September 30, 2021. For more information regarding PRF reporting requirements visit Reporting Requirements and Auditing | HHS.gov. If you would like assistance with this reporting contact one of our staff.
COVID-19 Accelerated and Advance Payment & Recover
CMS recently updated the COVID-19 Accelerated and Advance Payment Repayment & Recovery FAQS.
Click here for details from www.cms.gov.
Resources: Browser Support Changes for MCReF and PS&R, COVID-19 Vaccination Data Submission and MACs Resume
Resources Browser Support Changes for MCReF and PS&R
News from CGS: Beginning, Monday, June 21, 2021, the supported browser for MCReF and PS&R is changing from Microsoft Internet Explorer (IE) to Google Chrome. With this change, MCReF and PS&R will no longer actively support the IE browser.
Please work with your organization / IT support to ensure that you have access to Google Chrome on all devices necessary to continue using MCReF and PS&R.
COVID-19 Vaccination Data Submission
Effective May 21, 2021, nursing homes are required to report resident and staff vaccination information through the NHSN module per CMS' Interim Final Rule-3414. Any nursing homes that are not reporting this information weekly should do so immediately. Nursing homes that do not submit vaccination data for both residents and staff by 11:59pm June 13, 2021, will be imposed a civil money penalty. Furthermore, a higher civil money penalty will be imposed for each subsequent week that a facility does not report the required information.
For questions, please contact the CDC at: NHSN@cdc.gov
MACs Resume Medical Review on a Post-payment Basis
Beginning August 2020, Medicare Administrative Contractors (MACs) resumed post-payment reviews of items and services with dates of service before March 2020.
HHS Reporting Requirements
HHS revised the Post-Payment Notice of Reporting Requirements - PDF* as of June 11, 2021. There are now multiple reporting periods based on dates payments were received.
Click here for Reporting Requirements and Auditing details from HHS.gov.
Bed Reserve Reimbursement

Bed Reserve Reimbursement
CMS approved Kentucky State Plan Amendment (SPA) 21-0001. SPA 21-0001 provides for bed reserve reimbursement at 75% of the facility’s rate if the facility occupancy is 95% or greater for any census quarter of 2019.
Department of Medicaid Services (DMS) determined the reimbursement percentage for claims filed for bed reserve days with dates of service between the quarters of April 1, 2020 through June 30, 2021. Facilities that were eligible received a letter with updated Bed Reserve percentage for each quarter.
DMS processed the eligible bed reserve claims on Friday, June 4.
Do you have questions about the Bed Reserve Reimbursement? Call us with your questions at (270) 726-4033.
Blog by Sarah McIntosh, Director of Operations

Reporting Data to NHSN by June 13
Reporting Data to NHSN by June 13
CMS published an Interim Final Rule and a QSO that requires nursing homes to submit COVID-19 vaccination rates and treatments given to residents. CMS will start to enforce compliance and issuing Civil Money Penalties (CMPs) for facilities that did not report data to NHSN by midnight on June 13.
Click here to visit the CMS site.
Medicaid Rate Increased by $29
Medicaid Rate Increased by $29
CMS approved the Department for Medicaid Service’s request to increase Medicaid rate by $29 per day effective January 1, 2021 through the end of the quarter in which the Public Health Emergency (PHE) ends.
Accelerated and Advance Payments - Repayment Process Reminders

Accelerated and Advance Payments - Repayment Process Reminders
Providers who received an accelerated or advance payment during COVID-19 should have received a notification letter from CGS regarding the repayment process. The letter listed the advanced amount, the receivable transaction number and the repayment start date.
The Medicare remits will list the recoupments in the following format: WO/CVDAR000XXXXX
Click here to view the CGS Frequently Asked Questions.
Do you have questions about what this means for your facility? Call us with your questions at (270) 726-4033.
Blog by Kyle Fritsch, Billing Manager

Resources: KyHealthNet Updates
KyHealthNet Updates
You may or may not have noticed but KyHealthNet has not been allowing access to Account Management application. Facilities have not been able to edit user access, create new user access or change passwords prior to the expiration date. KyHealthNet now has a new link. You will need to make a new link and delete your old link.
Click here to visit the Kentucky Medicaid Site.
Program for Evaluating Payment Patterns Electronic Reports (PEPPER)
Program for Evaluating Payment Patterns Electronic Reports (PEPPER)
Fourth quarter fiscal year 2020 Program for Evaluating Payment Patterns Electronic Reports (PEPPERs) are available for Long-Term Care Hospitals (LTCHs), Critical Access Hospitals (CAHs), Inpatient Rehabilitation Facilities (IRFs), Inpatient Psychiatric Facilities (IPFs), hospices, and Skilled Nursing Facilities (SNFs).
Click here for guidance on accessing your report from www.pepper.cbrpepper.org.
Fiscal Year 2022 Skilled Nursing Facility Prospective Payment System Proposed Rule (CMS 1746-P)
Fiscal Year 2022 Skilled Nursing Facility Prospective Payment System Proposed Rule (CMS 1746-P)
• CMS estimates proposed rule that would result in increase of 1.3% to the Medicare rates for FY 2022.
• CMS is seeking comments on whether any necessary adjustment should be implemented to provide payment stability due to the PDPM not being budget neutral when implemented on October 1, 2019.
• CMS is proposing to suppress the SNF 30-Day All-Cause Readmission Measure for the FY 2022 SNF VBP Program. The reason is that circumstances caused by COVID-19 have affected the measure and the resulting scores.
Click here to view the related article to the aforementioned items.
KY Legislative Updates HB276 & HB278
House Bill 276
HB 276 passed out of the Senate today. 96-0 in house and 36-0 in Senate. HB 276 is an act relating to temporary personal care attendants transitioning to state registered nurse aides after the end of the public health emergency. HB 276 creates an “open door” for individuals who joined the long-term care workforce during the COVID-19 pandemic by recognizing their “on-the-job training” as a pathway toward certification as a nurse aide. Certified nurse aides are the backbone of the long-term care profession and the position is often the first step in the long-term care career ladder leading to jobs such as licensed practical nurses, registered nurses, directors of nursing, and corporate compliance.
HB 276 will now move to Governor Beshear to sign.
House Bill 278
HB 278, which made eligible expenses of an approved PPP loan deductible, was officially signed into law by Governor Beshear.
Thank you to everyone who reached out to their legislators on this bill. Your support helped get HB 278 across the finish line.
Resources: Tax Day Extension, 2021 Economic Impact Payment Status and more
Tax Day for Individuals Extended to May 17
Tax Day for individuals extended to May 17: Treasury, IRS extend filing and payment deadline The Treasury Department and Internal Revenue Service announced that the federal income tax filing due date for individuals for the 2020 tax year will be automatically extended from April 15, 2021, to May 17, 2021. Individual taxpayers can also postpone federal income tax payments for the 2020 tax year due on April 15, 2021, to May 17, 2021, without penalties and interest, regardless of the amount owed. This postponement applies to individual taxpayers, including individuals who pay self-employment tax. Penalties, interest and additions to tax will begin to accrue on any remaining unpaid balances as of May 17, 2021. Individual taxpayers will automatically avoid interest and penalties on the taxes paid by May 17. Individual taxpayers who need additional time to file beyond the May 17 deadline can request a filing extension until Oct. 15 by filing Form 4868. This relief does not apply to estimated tax payments that are due on April 15, 2021. These payments are still due on April 15.
Click here for additional details and updates.
2021 Economic Impact Payment Status Available
Find when and how the IRS sent your 2021 Economic Impact Payment with the Get My Payment tool.
UnitedHealthcare delegated to naviHealth
Most of you are familiar with naviHealth. Beginning April 1, 2021, UnitedHealthcare has delegated post-acute care management for UnitedHealthcare Medicare Advantage Members to naviHealth.
Please follow this link below for additional info.
Reminder: Kentucky Medicare Cost Report Filing Extension
Due to the COVID-19 public health emergency (PHE), the Centers for Medicare & Medicaid Services (CMS) delayed the cost report filing deadlines for all provider types with a fiscal year ending March 1, 2020 through December 31, 2020.
Please follow this link below for additional info.
PPP Deadline Extension
The Paycheck Protection Program (PPP) application deadline formally changed from March 31 to May 31.
Please follow this link below for additional info.
Medicare Credit Balance Quarterly Reminder
Reminder to submit the Quarterly Medicare Credit Balance Report by April 30, 2021, for the quarter ending March 31, 2021. Each provider must submit a quarterly Medicare Credit Balance Report (CMS-838) and certification for each PTAN.
Form CMS-838 is available here.
Fiscal Year (FY) 2022 Skilled Nursing Facility Prospective Payment System Proposed Rule (CMS 1746-P)
On April 8, 2021, the Centers for Medicare & Medicaid Services (CMS) issued a proposed rule that would update Medicare payment policies and rates for skilled nursing facilities under the Skilled Nursing Facility (SNF) prospective payment system (PPS) for fiscal year (FY) 2022. In addition, the proposed rule includes proposals for the SNF Quality Reporting Program (QRP), and the SNF Value-Based Program (VBP) for FY 2022. CMS is publishing this proposed rule consistent with the legal requirements to update Medicare payment policies for SNFs on an annual basis. The fact sheet discusses the major provisions of the proposed rule.
Click here to view the fact sheet.
KY Medicaid $29 Add-On

KY Medicaid $29 Add-On
HB192 includes a proposed $29 Medicaid Rate Add-On. Our state healthcare associations worked diligently to assure a State Plan Amendment was filed by March 31 requesting the add-on. These are the 4 areas covered:
• The add-on will be for all price-based nursing facility providers and will be effective January 1, 2021, once the SPA is approved and continue through the last day of the quarter in which the PHE ends or 12/31/21.
• The add-on will be applied to bed reserve days and, once the SPA is approved by CMS, days will be computed by increasing the facility rates by the $29 per day add-on, and then adjusting bed reserve rates by 50% or 75%, depending on the facility occupancy criteria.
• Providers will attest to expenditures only being used for PPE, COVID-19 testing, and staffing costs. Additional issues that may arise will be discussed in a future TAC meeting.
• The July 1st inflationary adjustment to the urban and rural price will be calculated first, followed by the addition of the $29 add-on to determine rates for Medicaid fiscal year 2022.
Do you have questions about what this means for your facility? Call us with your questions at (270) 726-4033.
Blog by Sarah McIntosh, Director of Operations

Medicare 2% Sequestration Cuts Delayed
Medicare 2% Sequestration Cuts Delayed
The House and Senate voted to delay the 2% across-the-board cut to Medicare through December 31, 2021. CMS has communicated there will be a temporary claims hold pending Congressional action to extend the 2% sequester reduction suspension. In anticipation of possible Congressional action to extend the 2% sequester reduction suspension, CMS instructed the Medicare Administrative Contractors (MACs) to hold all claims with dates of service on or after April 1, 2021, for a short period without affecting providers’ cash flow. This will minimize the volume of claims the MACs must reprocess if Congress extends the suspension; the MACs will automatically reprocess any claims paid with the reduction applied if necessary.
Do you have questions about what this means for your facility? Call us with your questions at (270) 726-4033.
Humana Reimbursement Switching from PDPM to Levels
Humana - PDPM to Levels
Humana is in the process of switching their reimbursement from PDPM to Levels. This change has occurred on 1/1/21 for some SNF’s and 6/1/21 for other SNF’s. For the SNF’s that have received notification from Humana regarding the reimbursement change at 1/1/21, we have noticed facilities receiving approvals at Level 1 or Level 2. Navihealth has approved some residents at Level 1 when they met Level 2 requirements. Please review your residents to ensure the level they are assigned is accurate and to avoid missing out on much needed revenue. Based on Humana’s standard level payments, the difference between Level 1 and Level 2 is $70 per day.
Do you think you might be missing out on revenue? Give us a call, we're happy to review.
Medicare B Credits
Medicare B Credits
You may have noticed your Medicare B payments were higher than your expected Accounts Receivable for January 2021. After reviewing multiple facilities, we confirmed overpayments are due to the 97535 HCPC code being paid in full when the MPPR should be applied. We will notify you once CMS and MAC’s implement a fix.
If you were a facility whose Medicare B payments were higher than the Accounts Receivable, we are available to discuss what your next steps should be.
Updates to SNF PDPM Claims
Updates to SNF PDPM Claims
MLN Matters MM11992 was recently published regarding a change to Medicare Claims Processing Manual, Chapter 6. The change addresses claims that are billed containing both covered days and noncovered days.
Economic Stimulus and Residents

Economic Stimulus and Residents
A very common question has been “if a nursing home patient receives a stimulus payment, will this affect Medicaid eligibility?” The Office of Inspector General recently published a newsletter with a link to a very helpful document published by NCLER. Please read the attached document to clear up any confusion.
If you would like clarity on how the stimulus payment may affect medicaid eligibility, contact us today.
Blog by Leah Shoulders, Billing Manager

Resources: CMS MLNMatters
CMS MLNMatters is discontinuing the MLN Products and MLN Matters electronic mailing lists.
Subscribe to your Medicare Administrative Contractor's (MAC) mailing list for all national and local Fee-For-Service (FFS) program news, including your MAC's news, MLN Connects® content, and MLN Matters® Article and MLN product updates.
Subscribe to our MLN Connects weekly email newsletter for all national FFS program news, including MLN Matters Article and MLN product updates.
Click here to subscribe to your Medicare Administrative Contractor's (MAC) Mailing List.
Click here to subscribe to our MLN Connects weekly email newsletter.
2021 Tax Filing Season Begins February 12
2021 Tax Filing Season Begins Feb. 12
The Internal Revenue Service announced that the nation's tax season will start on Friday, February 12, 2021, when the tax agency will begin accepting and processing 2020 tax year returns.
The February 12 start date for individual tax return filers allows the IRS time to do additional programming and testing of IRS systems following the December 27 tax law changes that provided a second round of Economic Impact Payments and other benefits.
This programming work is critical to ensuring IRS systems run smoothly. If filing season were opened without the correct programming in place, then there could be a delay in issuing refunds to taxpayers. These changes ensure that eligible people will receive any remaining stimulus money as a Recovery Rebate Credit when they file their 2020 tax return.
To speed refunds during the pandemic, the IRS urges taxpayers to file electronically with direct deposit as soon as they have the information they need. People can begin filing their tax returns immediately with tax software companies, including IRS Free File partners. These groups are starting to accept tax returns now, and the returns will be transmitted to the IRS starting February 12.
Click here to continue reading this information from IRS.gov.
SBA COVID-19 Funding Options
SBA COVID-19 Funding Options
The Paycheck Protection Program (PPP) is now offering Second Draw PPP Loans as well as First Draw PPP Loans for first time program participants. To find out if you qualify visit Paycheck Protection Program. SBA also offers other Coronavirus Relief Options, visit Coronavirus Relief Options to find out more or contact one of our staff to discuss.
If you have not filed your Loan Forgiveness Application for your first round PPP loan and would like assist contact us today.
HHS Reporting Requirements and Auditing

HHS Reporting Requirements and Auditing
Recipients of PRF payments exceeding $10,000 in aggregate must register in the Provider Relief Fund Reporting Portal. At present, there is no deadline for completing registration in the portal. Recipients will later receive a notification about when they should complete the second step of submitting reporting requirements information on the use of funds. HRSA will send a broadcast email to the email address you provide during the registration process. Below is the link for the portal registration.
If you would like assistance with the HHS reporting requirements or portal registration, please contact our office.
Blog by Sarah McIntosh, Director of Operations

Resources: 2021 Annual Update to the Therapy Code List, Prior Authorization and More
2021 Annual Update to the Therapy Code List
This MLN Matters Article is for physicians, therapists, providers, and suppliers billing Medicare Administrative Contractors (MACs) for therapy services provided to Medicare beneficiaries.
This article informs you of updates to the list of codes that sometimes or always describe therapy services. The additions, changes, and deletions to the therapy code list reflect those made in the Calendar Year (CY) 2021 CPT and Level II HCPCS. Make sure your billing staffs are aware of these updates.
Prior Authorization
Department for Medicaid Services mailed a provider letter dated January 7 regarding changes to the Ancillary Authorization Process.
Click here to view the provider letter. Click here to view the provider form.
ATTENTION ALL PROVIDERS: Effective with dates of service beginning 11/17/20, prior authorizations will be suspended for all provider types except for the following: EPSDT, Nursing Facility must continue to submit LOC via KLOCS and call Carewise Health at 1-800-807-8842 for ancillary services. Additionally, the 1915 c. Waivers - ABI, ABI LTC, Model II, SCL, HCB and Michelle P will require a prior authorization. Quality Incentive Payments If you have questions relative to the QIP payments, you should contact the following: HHS Increases and Begins Distributing Phase 3 Provider Relief Funding HHS Increases and Begins Distributing Over $24 Billion in Phase 3 COVID-19 Provider Relief Funding.
1. If you have issues with data submitted to the National Healthcare Safety Network, contact: NH_COVID_Data@cms.hhs.gov
2. If your data appears complete and you believe you have erroneously not received payment, you should contact: ProviderReliefContact@hrsa.gov
$900 Billion Stimulus Package

$900 Billion Stimulus Package
Congress passed the $900 billion Stimulus package. Highlights of what this means for Skilled Nursing Facilities is as follows:
• 2% sequestration relief extended thru March 31, 2021
• Some Medicare B cuts eliminated
• Budget vs Actual Lost Revenue calculations for Provider Relief Funds
The stimulus package is a mixed bag for the long term care sector. Learn more of what this bill means for Skilled Care Facilities.
Do you have questions about what this means for you? Call us with your questions at (270) 726-4033.
Blog by Sarah McIntosh, Director of Operations

2021 Medicare Part A & B Premiums and Deductibles
2021 Medicare Part A & B Premiums and Deductibles
On November 6, 2020, the Centers for Medicare & Medicaid Services (CMS) released the 2021 premiums, deductibles, and coinsurance amounts for the Medicare Part A and Part B programs.
• Skilled Nursing Facility coinsurance for 2021 - $185
• Medicare B deductible for 2021 - $203.00
Phase 3 Funding
Phase 3 Funding
In October 2020, Department of Health and Human Services (HHS) announced application process for Phase 3 funding of $20 billion. The application deadline was November 6, 2020. HHS has now decided to boost its Phase 3 funding total from $20 billion to $24.5 billion. HHS will be distributing the Phase 3 funding from December thru January 2021.
Kentucky is reported to receive $141 million of the $24.5 billion. Below is the reference.
Resources: COVID-19 Performance Payments and More
HHS awards nursing homes $523M in COVID-19 performance payments
HHS awards nursing homes $523M in COVID-19 performance payments Federal authorities announced that it will be distributing $523 million in the second round of performance payments. More than 9,000 nursing homes that have successfully reduced COVID-19-related infections and deaths between September and October will receive the payments. HHS found that 69% of the eligible facilities met the infection control criteria for the incentive program, while 68% met the mortality criteria.
CMS finalizes ‘shocking’ 9% therapy cuts, while affirming vast expansion of telehealth pay provisions
The Centers for Medicare & Medicaid Services formally announced Tuesday afternoon that it has finalized its calendar 2021 physician pay rule, which cuts physical, occupational and speech/language therapy payments for nursing homes patients by 9%.
Kentucky Medicaid - New Enrollment, Revalidation or Maintenance

Kentucky Medicaid - New Enrollment, Revalidation or Maintenance
Kentucky Department for Medicaid Services (DMS) has the Kentucky Medicaid Partner Portal Application (KY MPPA) system allowing all provider types to enroll, revalidate and/or perform maintenance electronically. Paper forms are NO longer accepted.
The KY MPPA system is available here.
The 2021 Provider Application Fee is $559 effective January 1, 2021.
If you need to make an update or revalidate your current Medicaid Provider information, such as license update, address change, EFT change, NPI/taxonomy change, change of ownership, name change, or revalidate you should use the KY MPPA system.
When Kentucky Medicaid providers update their licenses, they must submit a copy of the license to Kentucky Medicaid through KY MPPA to keep their provider information updated.
Blog by Sarah McIntosh, Director of Operations

3 Day Qualifying Stay and Benefit Period Waiver
3 Day Qualifying Stay and Benefit Period Waiver
These waivers have been renewed by the Secretary of Health and Human Services multiple times, most recently on October 2, 2020. Therefore, these waivers will continue to apply until at least January 20, 2021, unless the Secretary signs another extension of the PHE.
Testing for Long-Term Care Facilities - Modification
Testing for Long-Term Care Facilities - Modification
A contract was entered into by the Commonwealth of Kentucky and qualified vendors for COVID-19 Testing Services. This contract provides reimbursement to staff and residents of LTC for expenses incurred during the state of emergency. As of November 20, 2020, the Commonwealth of Kentucky received an additional $63M in federal funding. The revised contract amount is now $93M. The end date of the contract remains to be 12/30/2020.
Resources: Long Term Care Provider Newsletter, Joint Cybersecurity and More
KY Cabinet for Health & Family Services Office of Inspector General Division of Health Care Long Term Care Provider Newsletter
The Long Term Care Provider Newsletter published by the Cabinet for Health & Family Services Office of Inspector General Division of Health Care is a great resource for KY facilities.
Click here to view the October 2020 newsletter.
Joint Cybersecurity Advisory
CISA, FBI, and HHS have credible information of an increased and imminent cybercrime threat to U.S. hospitals and healthcare providers. CISA, FBI, and HHS are sharing this information to provide warning to healthcare providers to ensure that they take timely and reasonable precautions to protect their networks from these threats.
HHS Updates Provider Relief Fund FAQs
MLN Matters

MLN Matters
MLN Matters SE20011 was revised on 11/9/2020 to clarify the Skilled Nursing Facility (SNF) Benefit Period Waiver.
Statements worthy of reviewing regarding the Benefit Period Waiver:
1. Providers may utilize the additional 100 SNF days at any time within the SAME SPELL OF ILLNESS.
2. Ongoing skilled care in the SNF that is unrelated to the PHE does NOT qualify for the Benefit Period Waiver.
Click here to view the article.
Blog by Kyle Fritsch, Billing Manager

Medicaid Oxygen Fee Screens Based on DME Fee Schedule Amounts
Medicaid Oxygen Fee Screens Based on DME Fee Schedule Amounts
The Medicaid oxygen fee screens are based on the DME fee schedule amounts. The email below is from Cabinet for Health and Family Services and addresses the effective date for the oxygen fee screen amounts.
Each year Kentucky Medicaid is required to provide an Upper Payment Limit demonstration for CMS on DME codes covered by Kentucky Medicaid. This demonstration must reflect reimbursement rates for Kentucky Medicaid are set at or below the rates for the same codes listed by Medicare. Kentucky Medicaid was notified by CMS that we were out of compliance and must make adjustments to our fee schedule. To bring Kentucky Medicaid into compliance the Department for Medicaid Services immediately ordered a rate change adjustment to the 2020 DME fee schedule retroactive to 1/1/2020. This resulted in paid claims with any codes having rate decreases to automatically trigger a recoupment. The recoupment was in error. The recouped amounts will be reprocessed and repaid. Kentucky Medicaid apologizes for the late notice and any inconvenience that this has or may cause. The new effective date of the rates is 11/15/20.
Humana Medicare Advantage Change to Reimbursement Methodology
Humana Medicare Advantage Change to Reimbursement Methodology January 1, 2021
Humana recently mailed a letter to providers notifying them of their new payment methodology change effective January 1, 2021. Humana is changing the reimbursement methodology to Levels. Please see the attached memo and if you wish to object, notify Humana at the address listed in the memo.
Video: Medicaid Oxygen Reimbursement Change
Medicaid recently updated the oxygen reimbursement amounts the week of September 14th. The website states the oxygen reimbursement changes are effective 1/1/20. The reimbursement amounts are below and reflect the amounts listed on the website (link below). Watch Sarah's video for more details.
Click here for additional information.

In-Person Visitation Aid Grant Details
Civil Money Penalty (CMP) Reinvestment Application – In-Person Visitation Aids
The Centers for Medicare and Medicaid Services (CMS) recognizes that considerations allowing for visitation in each phase of re-opening may be difficult for residents and their families, CMS has developed this application template for request for the use of CMP funds to provide nursing homes with in-person visitation aids.
Funding for tents and Plexiglas (or similar product), are limited to a maximum of $3,000 per facility. Note, when installing tents, facilities must ensure appropriate Life Safety Code (LSC) requirements found at 42 CFR 483.90 are met, unless waived under the Public Health Emergency (PHE). All applicants must agree to the requirements defined in the project application.
Resources: Phase 3 Relief Details and More...
Trump Administration Announces $20 Billion in New Phase 3 Provider Relief Funding
Under this Phase 3 General Distribution allocation, providers that have already received Provider Relief Fund payments will be invited to apply for additional funding that considers financial losses and changes in operating expenses caused by the coronavirus. Previously ineligible providers, such as those who began practicing in 2020 will also be invited to apply, and an expanded group of behavioral health providers confronting the emergence of increased mental health and substance use issues exacerbated by the pandemic will also be eligible for relief payments.
How is the $2 billion incentive payment to skilled nursing facilities and nursing homes being determined?
In order for a facility to be eligible for payment, they must pass two initial gateway qualification tests on both their rate of infection and rate of mortality. First, a facility must demonstrate a rate of COVID infections that is below the rate of infection in the county in which they are located. This benchmark requirement for infection rate reflects the goal of the incentive program to recognize and reward facilities that establish a safer environment than the community in which they are located. Second, facilities must also have a COVID death rate that falls below a nationally established performance threshold for mortality among nursing home residents infected with COVID.
Public Health Emergency (PHE) Extension
Secretary Azar used his authority in the Public Health Service Act to declare a public health emergency (PHE) in the entire United States on January 31, 2020 giving us the flexibility to support our beneficiaries, effective January 27, 2020. The PHE was renewed on April 21, 2020, July 23, 2020, and October 2, 2020, effective October 23, 2020.
HHS Reporting Requirements Change as of September 19, 2020
This notice informs recipients of the categories of data elements that recipients must submit for calendar years 2019 and 2020 as part of the reporting process.
KY Medicaid Lab Fee Screen Amounts Updated
For SNF’s that have Medicaid only patients, Medicaid has recently updated the Lab fee screen amounts. SNF’s will need to update their software accordingly for the changed fee screen amounts.
Click here for the fee screen amounts.
Clarification on KY Medicaid add-on billing

Questions about the COVID-19 $270 add-on
There has been much discussion about billing Medicaid for COVID-19 patients and receiving the $270 add-on. The original FAQ document stated the Skilled Nursing Facility (SNF) had to receive a negative test result before the add-on billing ceased. There have been multiple discussions between SNFs due to the Office of Inspector General (OIG) stating residents were not required to be given the COVID-19 test to show a negative result.
Click here for clarification on Medicaid add-on billing.
Blog by Sarah McIntosh, Director of Operations

Hargis and Associates Team Members LeadingAge Virtual Conference Presenters
LeadingAge Kentucky 2020 Annual Conference
Join LeadingAge Kentucky for the 2020 Annual Conference on October 15-16, 2020. We'll have 2 team members as featured presenters during this virtual conference. More info on the conference coming soon!
Program Title: Make the Most of Your Provider Relief Funds: Tips to Successfully Account for Expenses
Date: October 15, 1:00-2:00 EST
Presenter: Sarah McIntosh, Director of Operations
Program Title: 7 Tips to Improve Your Accounts Receivable
Date: October 16, 10:30-11:30 EST
Presenter: Leah Shoulders, Billing Manager
Resources: IRS Notices, Nursing Home Relief and more
IRS temporarily stops mailing notices to taxpayers with balances due
The IRS has suspended the mailing of three notices – the CP501, the CP503 and the CP504 – that go to taxpayers who have a balance due on their taxes. Although the IRS continues to make significant reductions in the backlog of unopened mail that developed while most IRS operations were closed due to COVID-19, this temporary adjustment to processing is intended to lessen any possible confusion that might be associated with delays in processing correspondence received from taxpayers.
Trump Administration Announces $2 Billion Provider Relief Fund Nursing Home Incentive Payment Plans
Under the leadership of President Trump, the U.S. Department of Health and Human Services (HHS), through the Health Resources and Services Administration (HRSA), is announcing the details of a $2 billion Provider Relief Fund (PRF) performance-based incentive payment distribution to nursing homes. This distribution is the latest update in the previously announced $5 billion in planned support to nursing homes grappling with the impact of COVID-19. Last week, HHS announced it had delivered an additional $2.5 billion in payments to nursing homes to help with upfront COVID-19-related expenses for testing, staffing, and personal protective equipment (PPE) needs. Other resources are also being dedicated to support training, mentorship and safety improvements in nursing homes.
Nursing Home Infection Control Distribution

Infection Control Distribution is to be spent for costs associated with COVID-19
HHS distributed an initial $2.5 billion of the Nursing Home Infection Control Distribution funding on Thursday, August 27, 2020. Eligible nursing homes and skilled nursing facilities received a per-facility payment of $10,000 plus a per-bed payment of $1,450 in the first round of this distribution.
The Infection Control Distribution is to be spent for costs associated with administering COVID-19 testing for both staff and residents; reporting COVID-19 test results to local, state, or federal governments; hiring staff to provide patient care or administrative support; incurring expenses to improve infection control, including activities such as implementing infection control “mentorship” programs with subject matter experts, or changes made to physical facilities; and providing additional services to residents, such as technology that permits residents to connect with their families if the families are not able to visit in person.
Just like the other Provider Payment Relief payments, providers will have 90 days from receipt of payment to attest to the terms and conditions. The terms and conditions were wrongly placed under the link for the 2.5 billion SNF distribution.
Blog by Sarah McIntosh, Director of Operations

Kentucky COVID-19 testing, reimbursement, and support details
Get all the Kentucky COVID testing details, instructions, links and answers to your FAQs in this blog.
Kentucky COVID-19 testing, reimbursement, and support details:
To aid in advancing ongoing COVID-19 surveillance testing, the Kentucky Department for Public Health issued an order on July 9, 2020 indicating that a licensed clinician’s order is not required for a clinical laboratory to perform or bill for a COVID-19 FDA-approved diagnostic test. This guidance is intended to demonstrate Governor Andy Beshear’s continuing commitment to protect our most vulnerable citizens residing in Kentucky’s Long Term Care Facilities from COVID-19. Accordingly, effective immediately, the CHFS will continue its financial support of ongoing COVID-19 surveillance testing for residents and staff of LTC providers. The guidelines are based on what is currently known about the transmission and severity of COVID-19..
Details about testing, reimbursement, support and duration here. (Pdf)
Team Kentucky Reimbursement Instructions:
This contract is established to provide for reimbursement to providers, clinics and/or laboratories for testing costs of COVID-19 on non-insured and non-Medicaid eligible citizens of the Commonwealth, staff and residents of Long-Term Care Facilities, or any other population identified by the Secretary of the Cabinet for Health and Family Services.
Click here for details (pdf).
CHFS Surveillance COVID-19 Testing for Long-Term Care Facilities Frequently Asked Questions (FAQs):
Click here for details (pdf).
Resources: Flu Vaccines, Prior Authorization, and more
Apply Now: CARES ACT Provider Relief Fund Application Portal Now Open for Certain Medicare Providers
The U.S. Department of Health and Human Services (HHS) is distributing payments in the Phase 2 General Distribution of the Provider Relief Fund as part of ongoing efforts to offer financial relief to providers impacted by coronavirus disease 2019.
Allocations of CARES Act Provider Relief Fund for Nursing Homes
The Department of Health and Human Services (HHS), through the Health Resources and Services Administration (HRSA), is announcing the details of the next CARES Act-authorized nursing home Provider Relief Fund (PRF) distribution.
Flu Vaccine Amounts have been published for 2020-2021 Season
The Medicare Part B payment allowance limits for seasonal influenza and pneumococcal vaccines are 95% of the Average Wholesale Price (AWP) as reflected in the published compendia except where the vaccine is furnished in a hospital outpatient department. When the vaccine is furnished in the hospital outpatient department, payment for the vaccine is based on reasonable cost. Annual Part B deductible and coinsurance amounts do not apply for the influenza virus and the pneumococcal vaccinations. All physicians, non-physician practitioners, and suppliers who administer these vaccinations must take assignment on the claim for the vaccine.
PRIOR AUTHORIZATION TO RESUME AUG. 1st
Effective with dates of service beginning 8/1/2020, prior authorizations will resume with the exception of Behavioral Health and Substance Use Disorder (SUD) services. Behavioral Health and SUD services are defined as services provided by any Behavioral Health Provider type (02, 03, 04, 05, 06, 23, 26, 30, 62, 63, 66, 67, 81, 82, 83, 84, 89, 92), services listed on the Behavioral Health and Substance Abuse Services Inpatient and Outpatient fee schedules, and services listed on the Community Mental Health Center (CMHC) Mental Health Substance Abuse Codes and Units of Service fee schedule.
Medicare Payment Rates and SNF VBP Program Updates
Medicare payment rates and SNF VBP Program..
CMS issued final rule for Fiscal Year (FY) 2021 that updates Medicare payment rates and the value-based purchasing program for SNFs.
August Performance Score Reports now available to download
The August Performance Score Reports (PSRs) for the fiscal year (FY) 2021 Skilled Nursing Facility Value-Based Purchasing (SNF VBP) Program are now available to download. The PSRs provide SNFs with their performance information for the third year of the SNF VBP Program, including the incentive payment multiplier that will be applied to SNF Medicare fee-for-service claims from October 1, 2020 through September 30, 2021. The PSRs are distributed to SNFs via the Quality Improvement and Evaluation System (QIES) Certification and Survey Provider Enhanced Reports (CASPER) reporting system.
You may review illustrated steps for accessing your facility`s PSR here.
To receive your Medicare Rates for FY 2021, contact one of our client Managers today!
Flu and Pneumonia Billing in a Skilled Nursing Facility

Flu and Pneumonia Billing in a Skilled Nursing Facility (SNF)
For SNF’s, Medicare B pays for patients that receive the influenza, pneumococcal and Hepatitis B vaccines. As a reminder, the vaccines are a separate Part B inpatient benefit when rendered to beneficiaries in a covered Part A stay. Therefore, the SNF can be reimbursed for the vaccines given to all patients that have Medicare B, regardless if the patient is using Medicare A benefits or not.
Reference the Medicare Claims Processing Manual, Chapter 6, Section 20.4 for details.
Blog by Sarah McIntosh, Director of Operations

HHS Reporting Instructions
**BLOG UPDATED 8/18/2020: HHS delayed the additional details regarding the reporting instructions. HHS stated providers will receive detailed instructions and data template well before the reporting system’s October 1 availability.
Department of Health and Human Services (HHS) to release reporting instructions by August 17, 2020.
Provider Relief Fund (PRF) recipients that received one or more payments exceeding $10,000 will be required to submit future reports of how the PRF were spent.
• All recipients must report on their expenditures through December 31, 2020 by February 14, 2021.
• If there are remaining funds to be spent on December 31, 2020, a second and final report will be due July 31, 2021.
• Recipients who have expended all their funds prior to December 31, 2020 may submit a single report any time after October 1, 2020 but before February 15, 2021.
Deadline extended for providers to apply for the Medicaid & CHIP Provider Relief Fund
** BLOG UPDATED 8/6/20: This deadline has now been extended to August 28, 2020.
Dear Kentucky Medicaid & CHIP Leadership
I wanted to send you a note to follow up on the email that CMS sent out last Friday announcing HHS’ extension of the deadline for qualifying Medicaid & CHIP providers to apply for the Medicaid & CHIP Provider Relief Fund distribution.
CMS has been in continuous discussions with our partners at the Health Resources and Services Administration (HRSA) about the status of applications for this distribution. This email is intended to provide you with an update on the number of providers from your state that have applied.
As of July 15th, 143 qualifying Medicaid & CHIP eligible providers in Kentucky have applied for the Medicaid & CHIP Provider Relief Fund distribution out of the 22,751 providers identified in the data that your team supplied to CMS. Of these, 91 Medicaid & CHIP providers have been paid from this distribution. To ensure that all qualifying providers are aware of the opportunity, as well as the new application deadline, we are requesting that states reach out to your medical, dental, and long-term services and supports (LTSS) providers to remind them that they can begin the application process here.
To support these efforts, we’ve included below some resources that the HRSA team has released on the Provider Relief Fund that you can share:
Program Overview:
The bipartisan Coronavirus Aid, Relief, and Economic Security (CARES) Act and the Paycheck Protection Program and Health Care Enhancement Act provide $175 billion in relief funds to hospitals and other health care providers, including those on the front lines of the coronavirus response. A portion of these funds, under the Medicaid and Children’s Health Insurance Program (CHIP) Provider Distribution, provide help for providers and clinicians who treat our most vulnerable populations, including low-income and minority patients. This is allocated for eligible providers that participate in state Medicaid and CHIP Programs and that did not receive a payment from the Provider Relief Fund General Allocation. The payment to each provider will be approximately 2 percent of reported gross revenue from patient care.
Fact Sheet
The Health Resources & Services Administration (HRSA) released a Fact Sheet for Medicaid and CHIP Providers that is now available on the Provider Relief Fund website.
Recorded Webcast
A recording of the June 25 webcast is now available at https://www.hhs.gov/coronavirus/cares-act-provider-relief-fund/for-providers/index.html.
Frequently Asked Questions (FAQs)
In order to better address your most important concerns, HRSA has updated their FAQs to address common questions, including those submitted during the previous webcasts. The FAQs include expanded information on eligibility, application, payment process, and more.
Application Instructions
Medicaid and CHIP Provider Distribution Instructions and the Medicaid and CHIP Provider Distribution Application Form are available at hhs.gov/providerrelief. HRSA recommends downloading and reviewing these documents to help you complete the process through the Enhanced Provider Relief Fund Payment Portal.
Additional Information
For additional information, please call the Provider Support Line at (866) 569-3522; for TTY, dial 711. Hours of operation are 7 a.m. to 10 p.m. Central Time, Monday through Friday. Service staff members are available to provide real-time technical assistance, as well as service and payment support.
Summary of Provider Relief Fund Payments
Summary of Provider Relief Fund Payments.
General Distribution Payment:
Two separate payments on April 10-17 and April 24
Attestation deadline for April 10-17 payment was July 9
Attestation deadline for April 24 payment is July 23
Targeted SNF-Only Distribution:
Payment sent on May 22
Attestation deadline for May 22 payment is August 20
Targeted Medicaid/CHIP Distribution:
Eligible for Medicaid providers who have not received General Distribution payment
Applications must be submitted by July 20
Do I have to submit a quarterly report to HHS for April, May and June 2020 quarter?
No. All Recipients of the Provider Relief Fund payments who attest and agree to the Terms and Conditions, do not need to submit a separate quarterly report to HHS or the Pandemic Response Accountability Committee. HHS will submit a report containing all information necessary to comply with the reporting requirements of the CARES Act. However, HHS will be requiring recipients to submit future reports of how the Provider Relief Funds were spent. HHS will notify recipients of the content and due date.
What type of Documentation do I need to provide for the Provider Relief Fund Payments?
All expenses and lost revenues should be linked to COVID-19. Providers should not only track the expense but record what the item was used for and how it related to COVID-19. HHS has clarified that the Provider Relief Fund payments can be used for expenses incurred after January 1, 2020. These expenses must be related to COVID-19. HHS has said it will reconcile payments to expenses and lost revenues at the end of the pandemic.
What if I have excess Provider Relief Fund Payments that I do not spend?
HHS will provide directions on how to return the unused funds.
KENTUCKY LEVEL OF CARE SYSTEM (KLOCS)
KENTUCKY LEVEL OF CARE SYSTEM (KLOCS)
Starting August 3, 2020, all nursing and ICF/IID facilities will be required to use Kentucky Level of Care System (KLOCS) to submit Level of Care (LOC) applications and receive payment. Every facility will need a Kentucky Online Gateway (KOG) account to access KLOCS. Below is the TAKE ACTION NOW email that Department for Medicaid Services (DMS) has sent out.
Your facility must provide the Department for Medicaid Services (DMS) the names of individuals (2 max) responsible for managing your organization and its users in Kentucky Online Gateway (KOG). DMS will assign those individuals the KOG role of Organization Administrator. The Organization Administrator is responsible for granting and removing access to KLOCS on behalf of your organization.
How do I provide DMS this information?
Email KLOCSOrgAdmin@ky.gov the following information by 7/17/2020:
- Organization
- Name First and Last Name (2 people max per facility)
- Their email addresses
Guides for KOG Account Creation, the Organization Administrator Role, and Multi Factor Authentication (MFA) Set-Up will be available on the DMS KLOCS training page prior to the August 3, 2020 go-live.
What happens if my facility does not identify an Organization Administrator?
Without an Organization Administrator, your staff will NOT be able to access KLOCS to submit new LOC applications, initiate a request for PASRR Level II evaluations, nor manage active LOCs. This will impact your facility’s ability to receive payment.
If you have already provided DMS this information, please follow-up to confirm they received the initial request.
Resources: KLOCS, Medicaid Rates, PBJ and PDPM updates
Frequently Asked Questions about Taxation of Provider Relief Payments
The Coronavirus Aid, Relief, and Economic Security Act (CARES Act), enacted on March 27, 2020, appropriated $100 billion for the Public Health and Social Services Emergency Fund (Provider Relief Fund). The Paycheck Protection Program and Health Care Enhancement Act, enacted on April 24, 2020, appropriated an additional $75 billion to the Provider Relief Fund. This funding will be used to reimburse eligible health care providers for health care-related expenses or lost revenues that are attributable to the COVID-19 pandemic.
Kentucky Department for Medicaid Services Update on MDS Requirements
Effective October 1, 2020, Kentucky Medicaid will be requiring the reporting of the PDPM payment codes on the OBRA assessments when not combined with a 5‐day SNF PPS assessment.
Click to view the full details from Myers and Stauffer.
CMS plans to end the emergency blanket waiver
CMS announced plans to end the emergency blanket waiver requiring all nursing homes to resume submitting staffing data through the Payroll-Based Journal (PBJ) system by August 14, 2020. The memorandum also provides updates related to staffing and quality measures used on the Nursing Home Compare website and the Five Star Rating System.
Click here to visit the CMS website for details.
KLOCS Go-Live and Training
Kentucky Level-of-Care Systems (KLOCS) Go-Live and Training: AUGUST 3, 2020 Go to the following link for postings regarding web-based trainings.
Important Update: MEDICAID RATES - July 1
*Estimated Medicaid 1.5% Inflation Adjustment effective July 1, 2020
*DMS will not apply rate sanctions to the per diem rates effective July 1, 2020 and October 1, 2020, unless the Public Health Emergency ends prior to these dates.
CMS Issued an Emergency Grant Program

CMS Issued an Emergency Grant Program
CMS issued an emergency grant program, Communicative Technology Project, to assist in alleviating communication limitations due to COVID-19. Certified nursing facilities can apply for a Civil Money Penalty (CMP) fund grant for up to $3,000 to cover the costs of certain communicative technology devises and accessories.
Reminder that the CMP Grant opportunity is set to expire in July 2020.
Click here for the website and application.
Blog by Rhonda Houchens, Director of Operations

Resources: Kentucky Department for Medicaid Services Update on MDS Requirements
Kentucky Department for Medicaid Services Update on MDS Requirements
Click to view the full details from Myers and Stauffer.
Medicare Fee-for-Service (FFS) Response to the Public Health Emergency on the Coronavirus (COVID-19)
CMS provided clarification on provider utilization of the three day waiver and the benefit period waiver. Additional billing instructions have been provided for troublesome benefit period waiver claims.
Click here to visit the CMS website for details.
Provider Guidance: Phased Reduction of Restrictions for Long Term Care Facilities
This guidance is provided in accordance with the phased approach to resuming currently suspended services encouraged by the Centers for Medicare and Medicaid Services (CMS).
Resources: CMS-R-131
** BLOG UPDATED 8/6/20: Due to COVID-19 concerns, CMS is going to expand the deadline for use of the renewed ABN, Form CMS-R-131. The renewed ABN will be mandatory for use on 1/1/2021.
CMS-R-131
The ABN, Form CMS-R-131, and form instructions have been approved by the Office of Management and Budget (OMB) for renewal. The use of the renewed form with the expiration date of 06/30/2023 will be mandatory on 8/31/2020.
HHS - Medicare
HHS - Medicare
SIGN ATTESTATION
1. Have you completed Attestation Process via HHS website for Tranche 1, Tranche 2 and SNF Relief Fund Pmt?
2. Would you like for us to do this?
3. If yes, send the following info
- Tax ID Number
- Last 6 digits of Bank Account Number that money was deposited in
- Exact amount of Tranche 1 pmt, Tranche 2 pmt and - SNF Relief Fund Pmt
4. Sign the Attestation via the link: https://covid19.linkhealth.com/#/step/1
SUBMIT FINANCIAL DATA
1. Have you submitted Financial Data via HHS website? (Due by June 3, 2020)
2. Would you like for us to do this?
3. If yes, send the following info:
- Tax ID Number
- Last 6 digits of Bank Account Number that money was deposited in
- Exact amount of Tranche 1, Tranche 2 and SNF Relief Fund Pmt
- PD of most recently filed tax return to be uploaded
- Estimated Lost Revenue for March 2020
- Estimated Lost Revenue for April 2020
4. Submit your revenue information to be verified via the portal: https://covid19.linkhealth.com/#/step/1
TRACK HHS FUNDS
1. Do you want our assistance with HHS funds tracking?
2. Funds should be used on PREPARING, PREVENTING or RESPONDING to COVID-19
Contact us to learn more:
www.hargisandassociates.com
accountants@hargisandassociates.com
(270) 726-4033
CARES Act Provider Relief Fund

What is eligible for reimbursement?
HHS has distributed money to SNFs to help them combat the devastating effects of this pandemic. A very common question has been, “What expenses or lost revenues are considered eligible for reimbursement?”
The HHS.gov website has a shared a list of Frequently Asked Questions concerning the CARES Act Provider Relief Fund, including a response to this question on page 6.
Blog by Sarah McIntosh, Director of Operations

Resources: HHS Relief for Skilled Nursing Facilities (SNFs)
HHS Releases $4.9 billion in COVID-19 Relief for Skilled Nursing Facilities (SNFs)
SNFs received a baseline payment of $50,000, plus an additional $2,500 per bed.
As with other rounds of CARES Act funding, SNFs must agree to the terms and conditions in order to accept the cash.
SNF’s must also comply with future audit and reporting rules. Below is the link to the terms and conditions posted on HHS website.
Click here to view the HHS website.
Articles referencing Relief funds:
Click here to learn more from McKnights Long-Term Care News.
Small Business Administration (SBA) Payroll Protection Program (PPP)
Small Business Administration (SBA) Payroll Protection Program (PPP)
Every borrower should begin preparing for the loan forgiveness process. Make sure that you are documenting how you spend you PPP proceeds and have proper documentation.
Below is a list of some information that will be needed:
• The number of full-time equivalent (FTE) employees on your payroll as of the following time periods
1. 8 week “covered period”
2. 2/15/19 to 6/30/19
3. 1/1/20 to 2/29/20
• Dollar amount of Payroll cost during the “covered period”
• Dollar amount of non-payroll cost incurred during the “covered period”
• Did you receive an SBA Economic Injury Disaster Loan (EIDL)
The Department of Health & Human Services
HHS Provider Letters
The Department of Health & Human Services recently sent letters to providers regarding submitting revenue data to the General Distribution Provider Portal for verification. The letter states “All providers, including those paid based on the revenue data already submitted in CMS cost reports, are required under the Terms and Conditions to submit revenue information to the General Distribution Provider Portal for verification.“
There has been much confusion if Providers are required to submit their revenue information. The provider letter states that ALL providers must submit their revenue information. Click here to view the Provider Letter.
Steps all Providers need to complete:
1. Sign the Attestation via the link: https://covid19.linkhealth.com/#/step/1
Info needed:
A. Tax ID number
B. Last Six Digits of Bank Account Number
C. Exact amount of the Relief Fund Payment
2. Submit your revenue information to be verified via the portal: https://covid19.linkhealth.com/docusign/#/step/1
Info needed:
A. Tax ID number
B. Last Six Digits of Bank Account Number
C. Exact amount of the Relief Fund Payment
D. Gross receipts of sales
a. Box 1a of IRS Form 1120
b. Box 1a of IRS Form 1120S
c. Box 1a of IRS Form 1065
d. Part I, 9 “Program Services Revenue” of IRS Form 990
E. Estimated Lost Revenue for March 2020
F. Estimated Lost Revenue for April 2020
G. Copy of IRS Form 1120 to upload
Resources: Relief Programs, CMS and Medicaid Updates
CARES Act Provider Relief Fund
President Trump is providing support to healthcare providers fighting the COVID-19 pandemic through the bipartisan CARES Act and the Paycheck Protection Program and Health Care Enhancement Act that provide $175 billion in relief funds to hospitals and other healthcare providers on the front lines of the coronavirus response. This funding supports healthcare-related expenses or lost revenue attributable to COVID-19 and ensures uninsured Americans can get testing and treatment for COVID-19.
Nursing Home Five Star Quality Rating System updates, Nursing Home Staff Counts, and Frequently Asked Questions
CMS is committed to taking critical steps to ensure America’s nursing homes are prepared to respond to the threat of the COVID-19.
Nursing Home Compare website & Nursing Home Five Star Quality Rating System: We are announcing that the inspection domain will be held constant temporarily due to the prioritization and suspension of certain surveys, to ensure the rating system reflects fair information for consumers.
Posting of surveys: CMS will post a list of the surveys conducted after the prioritization of certain surveys, and their findings, through a link on the Nursing Home Compare website.
Nursing Home Staff: CMS is publishing a list of the average number of nursing and total staff that work onsite in each nursing home, each day. This information can be used to help direct adequate personal protective equipment (PPE) and testing to nursing homes.
Frequently Asked Questions (FAQ): We are releasing a list of FAQs to clarify certain actions we have taken related to visitation, surveys, waivers, and other guidance.
CMS Reevaluates Accelerated Payment Program and Suspends Advance Payment Program
On April 26, 2020, the Centers for Medicare & Medicaid Services (CMS) announced that it is reevaluating the amounts that will be paid under its Accelerated Payment Program and suspending its Advance Payment Program to Part B suppliers effective immediately. The agency made this announcement following the successful payment of over $100 billion to healthcare providers and suppliers through these programs and in light of the $175 billion recently appropriated for healthcare provider relief payments.
Kentucky News
See the latest news and updates from Governor Beshear.
MEDICAID PROVIDER LETTER
This memo from the Kentucky Department for Medicaid Services gives details for the following updates.
Effective April 1, 2020, Medicaid Rate add-on of $270 for COVID-19 positive patients.
Effective April 24, 2020, Medicaid is implementing a temporary process for Medicaid eligibility.
Effective April 1, 2020 Medicaid will be increasing the bed reservation days to 30 per calendar year through the state of emergency.
Resources: Long Term Care Provider News
COVID-19 Emergency Circumstances LTC Bed Change Requests
As a result of the COVID-19 pandemic, CMS has demonstrated unprecedented flexibility to long-term care facilities in order to protect residents during the pandemic. CMS has released the “COVID-19 Long-Term Care Facility Guidance”, issued blanket waivers for certain CMS requirements of participation for LTC facilities, as well as offered flexibility regarding timeframes for COVID-19 emergency bed change requests. In response to the relaxed requirements offered by CMS and Governor Andy Beshear’s Executive Order 2020-215 declaring a state of emergency in the Commonwealth, a new bed change request process has been developed. The COVID-19 Emergency Circumstances LTC Bed Change Request Process allows for the faster processing of temporary bed change requests due to emergency circumstances related to the COVID-19 pandemic. This process waives all licensure and architectural review fees, allows for architectural desk reviews, removes the typical CMS timeframe requirements and eliminates the requirement for color coded floor plans when requesting certification status changes.
Emergency CMP Grant Project
It is with great pleasure that the Cabinet for Health & Family Services (CHFS) announces an emergency Civil Money Penalty (CMP) Grant Project opportunity for all certified nursing facilities within the Commonwealth. Specifically, CMS has notified the CHFS office that a grant program, Communicative Technology Project, has been approved to assist in alleviating communication limitations due to COVID-19. This grant program will allow Medicare-certified nursing facilities to apply for a CMP fund grant for up to $3,000 to cover the costs of certain communicative technology devices and accessories. More information can be found on the OIG Civil Money Penalty Funds website.
Department for Medicaid Services Update on Optional State Assessment
On March 19, 2020, CMS announced that changes to the Minimum Data Set (MDS) 3.0 v1.18.1 are being delayed, therefore, an Optional State Assessment (OSA) is not needed on October 1, 2020, as originally anticipated, in order to continue Resource Utilization Group (RUG) based Medicaid reimbursement.
We continue to expect that in the future, CMS will remove items from the MDS item set that are needed for maintaining RUG case mix reimbursement. As CMS modifies the items on the MDS assessments in the future, DMS will evaluate if OSAs will be needed to continue its RUG‐III reimbursement system. Communications regarding any future OSA requirement will be issued at that time. We will continue to publish information as it becomes available.
Should you have any questions, please contact Jacob Wilson at (502) 564-8196, extension 2103. Questions regarding the coding of the MDS assessments may be directed to Chrystal Daugherty, RAI Coordinator with the Office of Inspector General at 606-330-2030, extension 283.
PDPM v1.0004
A revision to the PDPM DLL Package (V1.0004 FINAL) was posted, and the previous version (V1.0003 FINAL) was removed. This version adds support for the new ICD-10-CM code for Coronavirus, U07.1. Note that this code is ONLY in effect for assessments with target date 04-01-2020 and later. The package contains updated test files and documentation.
Also, the lookup file for the allowable ICD codes in item I0020B has been updated to include U07.1, and it is posted as a separate ZIP file. Again, please note that this code is ONLY in effect for assessments with target date 04-01-2020 and later. The files are located in the Downloads section of the MDS 3.0 Technical Information site.
Audits are the new normal.

Audits are the new normal
CMS uses Comprehensive Error Rate Testing (CERT) audits to see if MACs are properly paying claims. CERT audits focus on logistical issues, such as whether or not the coding and billing are correct. CERT is looking for errors in payments made by carriers. Providers are affected because the CERT looks into a claim via Medical Records request. If the CERT uncovers an error, the CERT will recoup money from the provider. CERTs receive set amount outlined in their contract, regardless of the amount of payment errors they find.
Recovery Audit Contractors focus on errors created by the providers. The primary purpose of RAC is to detect and correct improper payments. RACs are paid through contingency fees (money they uncover). The contingency fee payment system encourages RACs to find errors.
Zone Program Integrity Contractors (ZPICs) are the most complex audits. ZPICs compare providers billing with similar providers. ZPIC reviews are not random. They are conducted under a presumption of fraud. ZPICs can be initiated by data analysis, frequency, whistleblowers or referred by MACs. Once an error is found they extrapolate the data in order to determine the amount of misappropriated funds.
Blog by Sarah McIntosh, Director of Operations

Resources and Important Updates: Medicaid
MEDICAID
All DCBS offices are closed for appointments. Individuals may apply for Medicaid by calling the Kentucky Healthcare Customer Service line at (855)459-6328, visit the Benefind website (benefind.ky.gov) or by calling the DCBS Call Center at (855)306-8959.
During the COVID-19 State of Emergency, individuals who need special healthcare coverage should go to the kycovid19.ky.gov website and click on Services. The special healthcare coverage is temporary and ends on 06/30/2020 unless an application for regular Medicaid is submitted.
Resources and Important Updates
CARES ACT Provider Relief Fund to infuse $30 billion into healthcare system.
All facilities and providers that received Medicare fee-for-service (FFS) reimbursements in 2019 are eligible for this initial rapid distribution. These are payments, not loans, to healthcare providers, and will not need to be repaid. The payments should be arriving via direct deposit beginning April 10, 2020.
Fiscal Year 2021 Proposed Medicare Payment and Policy Changes
CMS projects aggregate payments to SNFs will increase by $784 million, or 2.3 percent, for FY 2021 compared to FY 2020.
Kentucky and Ohio Part A News from CGS
CGS is aware that certain eligible provider types may not have received the maximum eligible amount for their accelerated payment. We are identifying providers impacted by the 3-6 month max issue and determining a resolution. Please continue to monitor the CPIL for updates.
Kentucky Department for Medicaid Services Update on Cost Report Extensions
CMS has directed MAC's to further extend the cost reporting deadlines for the following cost reporting fiscal year ends (FYE) for all provider types:
Cost Reporting Period Ending -- Extended Due Date
10/31/2019 -- 06/30/2020
11/30/2019 -- 06/30/2020
12/31/2019 -- 08/31/2020*
01/31/2020 -- 08/31/2020*
02/29/2020 -- 09/30/2020*
*Please note, these are new extensions.
While we have been told that CMS is considering the 03/31/2020 FYE providers that are currently due 08/31/2020, no extension has been posted at this time.
The Advance Beneficiary Notice of Noncoverage
The Advance Beneficiary Notice of Noncoverage (ABN) Form CMS-R-131 is issued by providers to Original Medicare beneficiaries when Medicare payment is expected to be denied. Skilled Nursing Facilities (SNFs) issue the ABN to transfer potential financial liability for items/services expected to be denied under Medicare Part B only.
Form CMS-R-131, will expire 03/2020. The form is currently awaiting OMB approval for renewal. CMS will provide instructions when it does get approved. In the meantime, continue to use the current form until further instruction is provided.
CMS Flexibilities to Fight COVID-19
CMS is waiving 42 CFR 483.70(q) to provide relief to long term care facilities on the requirements for submitting staffing data through the Payroll-Based Journal system.
Tracking COVID-19 Related Costs
![]()
COVID-19 Expenses
In this unprecedented time, our firm strongly recommends that all additional costs, related to COVID-19, be tracked separately from all other costs/departments. We recommend setting up a "new" department in your general ledger (financial statements) to track as many COVID-19 related expenses as possible. In these uncertain times, we want to be cautious and proactive. Facilities might have to verify the additional costs due to, but not limited, to the following.
Loans (SBA and others) - example: 8 week tracking period for SBA loan
Potential Medicaid additional add-ons (currently under discussions)
Others
Below are examples of possible additional expenses:
Payroll - example: new staff hired for infection control, replacement workers for those sick, OT, additional labor for cleaning, hazard pay to maintain staff, etc.
Personal Protective Equipment (PPE) - masks, gloves
Screening costs for employees to enter the building
Cleaning supplies and additional costs for everyday supplies
Building retro fittings - example: putting in dividers to separate employees, staff, etc.
Please inform those responsible for your general ledger/financial statements. If you have any questions or need assistance, please contact our office.
Blog by Robin Parker, CPA, Sr. Accountant

RESOURCES: Important Updates Concerning COVID-19
IMPORTANT UPDATE: From UnitedHealthcare
Suspension of prior authorization requirements to a post-acute care setting through May 31, 2020. Details: Waiving prior authorization for admissions to: long-term care acute facilities (LTAC), acute inpatient rehabilitation (AIR), and skilled nursing facilities (SNF). Consistent with existing policy, the admitting provider must notify us within 48 hours of transfer and penalties still apply. Length of stay reviews still apply, including denials for days that exceed approved length. Discharges to home health will not require prior authorization. Prior authorization is not required for COVID-19 testing and COVID-19 testing related visits.
IMPORTANT UPDATE: From Anthem Blue Cross Blue Shield
Anthem is committed to working with and supporting providers. As of March 16, Anthem is removing prior authorization requirements for skilled nursing facilities (SNF) for the next 90 days to assist hospitals in managing possible capacity issues. SNF Providers should continue admission notification to Anthem in an effort to verify eligibility and benefits for all members prior to rendering services and to assist with ensuring timely payments. In addition, Anthem is also extending the length of time a prior authorization is in effect for elective inpatient and outpatient procedures to 90 days. This will help prevent the need for additional outreach to Anthem to adjust the date of service covered by the authorization. This applies to members of all lines of business, as well as self-insured plan members.
Kentucky Medicaid COVID-19 Information - Cabinet for Health and Family Services
The information on this page is specific to Medicaid beneficiaries and providers. For more information about COVID-19, refer to the state COVID-19 website.
UPDATE: KLOCS Training
More information will be provided when the new "go-live date" is determined and training forums are rescheduled. Thank you for your understanding as well as your continued commitment to keep your communities and residents safe.
Reference from PointClickCare: COVID-19 CMS Medicare Waivers
COVID-19 CMS Medicare Waivers
3/19/2020
Attention all Financial and Billing Staff
On March 13, 2020 the Centers for Medicare and Medicaid Services (CMS) issued a blanket waiver based on the declared public health emergency (PHE) COVID-19. This includes waivers for:
• 3 day qualifying hospital stay
• 60 day break in spell of illness. This extends an additional 100 day benefit period for residents who have recently exhausted Skilled Nursing benefits and must remain in a facility.
To view the full communication from CMS, click here.
PointClickCare is currently in communication with CMS to clarify billing and MDS requirements surrounding these waivers. To prepare for monthly billing, review the COVID-19 Waiver Billing Quick Reference Guide (QRG).
PointClickCare is currently working to bypass the UB Edit Check of missing occurrence span code 70 Qualifying Hospital Stay or the demonstration code if DR is on the claim. Continue to monitor the Home Page for more information.
Click here to view the COVID-19 Waiver Billing Quick Reference Guide (QRG) from PointClickCare.
If your SNF needs assistance with this setup, please contact our office.
SNF Coronavirus waiver
President Trump declared a national emergency on March 13, 2020. CMS issued Coronavirus 1812(f) waiver of the 3-Day Stay inpatient hospital requirement for Skilled Nursing Facilities (SNF). According to Administrator Verma’s press conference on March 13, 2020, the waiver takes effect retroactively to March 1, 2020. https://www.cms.gov/newsroom/press-releases/emergency-declaration-press-call-remarks-cms-administrator-seema-verma
FAQ link from CMS. https://www.cms.gov/About-CMS/Agency-Information/Emergency/Downloads/MedicareFFS-EmergencyQsAs1135Waiver.pdf

For billing under this waiver, the Disaster Related (DR) condition code should be used by SNFs (institutional providers). The DR condition code is used at the claim level when all of the services billed on the claim are related to the emergency/disaster. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c38.pdf
PLEASE NOTE THAT AN ADMITTING RESIDENT MUST MEET SKILLED CRITERIA IN CHAPTER 8 OF THE MEDICARE BENEFIT POLICY MANUAL. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c08pdf.pdf
COVID-19 MEMO
Hargis & Associates (H&A) places the health and safety of our clients, employees, and our health care community as our highest concern. As we continue to serve you, we are continuously monitoring the growing COVID-19 situation and those recommendations from World Health Organization (WHO) and the Center for Disease Control & Prevention (CDC).
At the present time, H&A has not experienced any interruption to our services or hours. We are encouraging all clients and employees to practice safe measures regarding health including cleaning for disinfection, hand washing, stay home if you are sick, limiting exposure, etc.
H&A is diligently reviewing all CMS and State guidance affecting health care coverage, billing and coding, and payment to our clients.
Please reference this CMS link for current guidance on these issues: https://www.cms.gov/About-CMS/Agency-Information/Emergency/EPRO/Current- Emergencies/Current-Emergencies-page
H&A recognizes the hardships you may be facing as a result of the COVID-19. We strive to continue to offer our services during these challenging times. If you find yourself needing assistance with billing or accounting functions due to staff shortages or the need to have all hands-on deck at your facility, please don’t hesitate to reach out to us for help. We are here to serve our elderly population every day and especially in times of crisis.
H&A will provide updates regarding the above to our clients and health care community through numerous avenues including publications at our office, our website, social media, etc. For more information or assistance visit our website or call our office.
Recurring Quarterly Submissions That SNFs Are Required to File
PBJ & Credit Balance Reports
Staffing Data Submission Payroll Based Journal (PBJ)
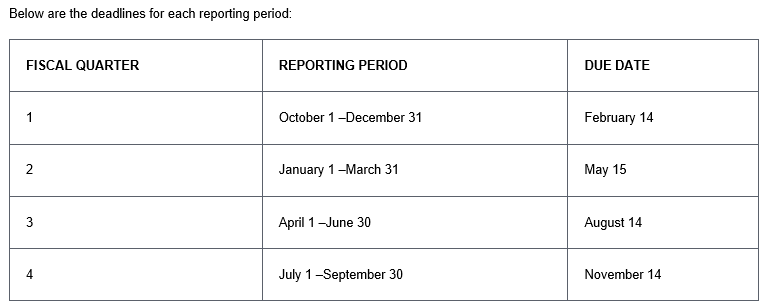
Credit Balance Report (Form CMS-838)
A Medicare credit balance is an amount determined to b refundable to the Medicare program for an improper or excess payment made to a provider because of patient billing or claims processing errors. Each provider must submit a quarterly Credit Balance Report (Form CMS-838) If your facility has more than one provider number, a separate report should be submitted for each provider number. If you fail to submit a Credit Balance (CMS-838) form and/or certification page with all provider numbers identified, Medicare payments will be suspended as stated in 42 CFR 413.20(e) and 405.370. Providers with low Medicare utilization, as specified in the Provider Reimbursement Manual, CMS Pub. 15-1, Chapter 24 2414.4 B, or who file less than twenty-five Medicare claims per year, do not have to submit Form CMS 838. Providers that qualify should submit one, signed and dated certification page and a letter indicating that they are a low Medicare utilization provider. The following provides the reporting periods and associated due dates.
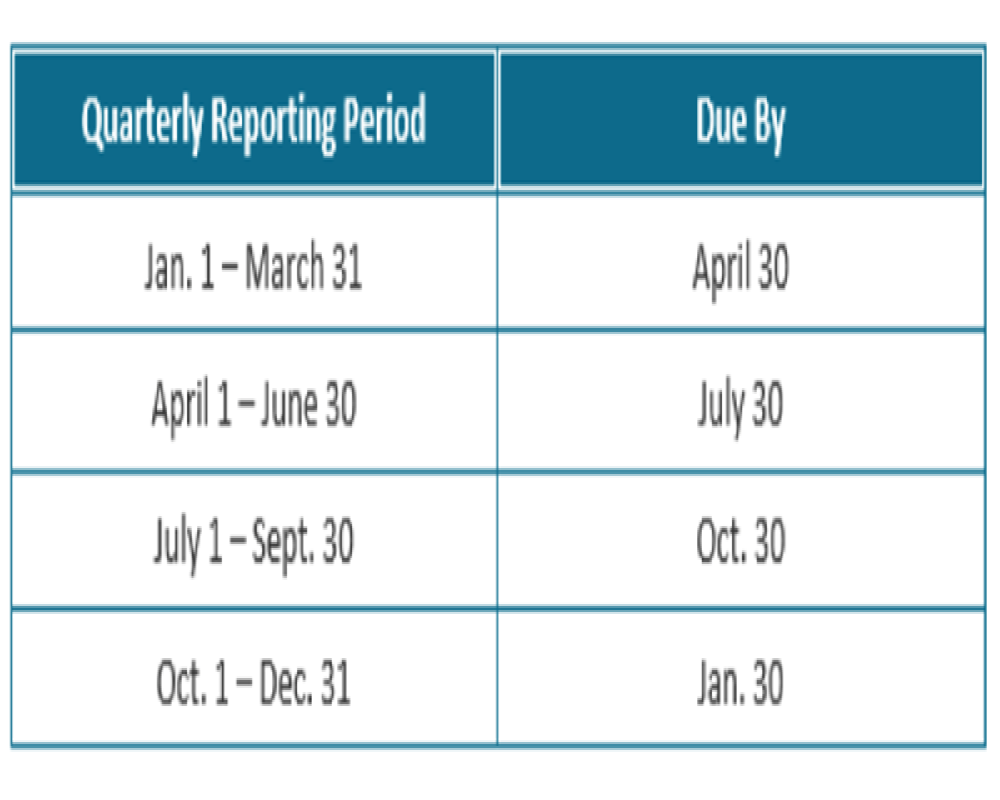
Has your facility received a letter from Alliant Health Solutions?

Quality Improvement Organizations (QIO)
Some nursing facilities have received a letter from Alliant Health Solutions and are questioning if Alliant is replacing KEPRO. KEPRO is the CMS Beneficiary and Family Centered Care – Quality Improvement Organization (BFCC-QIO) for Kentucky. KEPRO assist Medicare patients in exercising their right to appeal discontinued Medicare benefits. KEPRO remains to be Kentucky’s BFCC-QIO.
Alliant is CMS Quality Innovation Network – Quality Improvement Organization (QIN-QIO). The QIN-QIO is responsible for working with health care providers and the community on data-driven projects to improve patient safety, reduce harm and improve clinical care at the local level.
Click here for a reference to help providers to locate the BFCC-QIO and the QIN-QIO for each state.
Blog by Sarah W. McIntosh, Director of Operations

Don't Overlook Tax Credits & Incentives!
Build a Better Bottom Line with Our Tax Solutions
Our Services - Tax
Manage your tax department with the knowledge needed to efficiently and effectively build a better bottom line with our tax solutions. Reduce the risk of overlooking tax credits and incentives. Hargis & Associates works for your business to identify opportunities resulting in optimal tax savings. We do the work for you; saving you time and resources.
Our dedicated and experienced staff successfully works with your team and the IRS during any tax auditing process. Faithfully rely on us to provide value-added insight.
Hot Topics
Hot Topics
A few Hot Topics in the news.
Publication of FY 2022 SNF Annual Payment Update (APU) Overview Table (Click here to read.)
CMS posts MDS 3.0 QM User’s Manual V13.0, Quality Measure Reporting Module Table V1.8 (Click here to read.)
2020 Physicians fee schedule has been revised (Click here to read.)
IRS Creates New, Large Print Tax Form for Seniors (Click here to read.)
New Inspector General named (Click here to read.)
MACs will bypass the edit that requires an occurrence code 50 AND update the edit that ensures the default HIPPS code (Click here to read.)
Publication of FY 2022 SNF Annual Payment Update (APU) Overview Table
Publication of FY 2022 SNF Annual Payment Update (APU) Overview Table
Article from Centers for Medicare & Medicaid Services (CMS)
CMS published the FY 2022 SNF Annual Payment Update (APU) table. This table indicates the data elements CMS will use for FY 2022 SNF QRP APU determinations. The SNF APU table is available in the document titled “FY-2022-SNF-QRP-APU-Table-for-Reporting-Assessment-Based-Measures-and-SPADEs-Finalized.pdf” in the Downloads section of the SNF Quality Reporting Program Measures and Technical Information webpage.
Click here to view the FY 2022 SNF Annual Payment Update (APU) table.
Coding for HIV/AIDS Patient

Coding for HIV/AIDS Patient
When billing Medicare A it is important to make sure you are checking your diagnosis when you have an HIV/AIDS patient. That diagnosis needs to be present on the claim in the first 9 diagnosis or you could miss that extra reimbursement. For example, a resident with HIPPS KAXD would be paid roughly $4500 for 9 days. With the AIDS NTA bump and Nursing addon, the reimbursement increases to $6,426.18.
Click here to view the CMS website, under Fact Sheet, PDPM Payments for SNF Patients with HIV/AIDS.
Unlike other healthcare tax accounting firms, Hargis & Associates, LLC has a widely respected reimbursement team. We are dedicated to being on the forefront of the ever-changing financial climate. We understand the need for billing, training and accounts receivables management facing nursing facilities; that is why we ease the process through our advanced, healthcare billing department. With our proven billing services in place, clients improve cash flow by reducing days in outstanding accounts receivables.
Our Billing Services Include:
• Medicare A & B Billing
• Medicaid Billing
• Medicare Replacement/Managed Care Billing
• Medicare A and B Co-Insurance Billing
• Hospice Billing
• Filing of Medicare Credit Balance Report
• Medicare Bad Debt Log for Cost Report
• Online Billing Analysis, Rebilling, and Collections
• Posting of Cash receipts, adjustments, etc.
• Posting of Ancillary charges
• Accounts Receivable Analysis
• Appeals
• On-Site Training
• Billing Assistance Program
Blog by Leah Shoulders, Billing Manager

Updated Five-Star Ratings Released Today
Updated Five-Star Ratings Released Today
Article from LongTermCareLeader.com
NHC is usually updated the fourth Wednesday of every month, but the updates on the first month of the quarter (i.e. January, April, July, October) are more noteworthy. They include updated quality and staffing data. Other monthly updates only include updated survey data.
- Quality Measure Data for 2018-Q4 to 2019-Q3 (Oct’18 – Sep’19) Released
- Payroll-Based Journal (PBJ) Staffing Data for 2019-Q3 (Jul’19 – Sep’19) Released
- Table of Expected Nursing Home Compare Releases with Updated Quality and Staffing Data in 2020
- Expect This Newer Data on LTC Trend Tracker Within a Week




